Addiction treatment organizations in Ohio are most likely to run across plans issued by Medical Mutual of Ohio, Anthem Blue Cross and Blue Shield in Ohio, Aetna Inc, United HealthCare of Ohio, Caresource Management Group, Molina Healthcare Inc, Buckeye Community Health Plan and Paramount Advantage.
Answers to Your Top Questions About Addiction Treatment Billing in Illinois
How to Turn Your Group Practice Into an Outpatient Facility Offering IOP or PHP in New York
Your Complete Addiction Treatment Billing Guide to New York
Your Complete Guide to Addiction Treatment Insurance Billing in Florida
What Are the Most Used Addiction Treatment CPT Codes in Texas?
Our Top 5 Tips for Addiction Treatment Insurance Billing in California
Looking for the Expedited Appeal Line for Anthem, Inc. Addiction Recovery Claims?
Here's How to Find the Addiction Treatment Billing Claims Address for Blue Cross Blue Shield of Minnesota
Where to Find Addiction Treatment Billing Contact Information for Blue Cross Blue Shield of Massachusetts
Blue Cross MA provides ample information about how to submit original claims on their website. Medical providers - like behavioral healthcare professionals and addiction treatment clinics and centers - can contact provider services for claims, as well. The number to use depends on the nature of your organization.
Where Can I Find Addiction Treatment Utilization Forms for Premera Blue Cross?
What Reviews are Required for Addiction Treatment Providers Under Blue Cross Blue Shield of Tennessee?
Top 5 Addiction Treatment Diagnosis Codes to Use for URs with Healthfirst Insurance
What Addiction Treatment CPT Codes Require Pre-Certification at Highmark, Inc.?
Understanding CareSource Management Group's Shareable Client Information Policies for Addiction Treatment
Where to Find Addiction Treatment Utilization Forms for L.A. Care Health Plan
How to Complete Insurance Registration with Florida Blue for Addiction Treatment Centers
How to Complete Registration as a Provider or Pharmacy with Express Scripts, Inc. for Addiction Treatment Centers
Express Scripts is the largest pharmacy benefit management organization in the United States. It also operates one of the nation’s largest by-mail pharmacies. Over 85 million people receive pharmacy coverage through Express Scripts. The company counts revenues in excess of $100 billion per year. Express Scripts works with many different health insurance payers - government plans, employer plans, and personal plans - to cover the pharmaceutical piece of health insurance. Express Scripts was acquired in recent years by Cigna, and is also associated with Evernorth, a Cigna company.
How to Work with Addiction Treatment Patients Who are Express Scripts Members
There are several situations where an addiction treatment center may need to deal with medical billing for Express Scripts.
The main Express Scripts-related situation most addiction treatment providers will encounter is when an addiction treatment center offers Medication Assisted Treatment (or MAT) for patients in addition to other types of behavioral health services. Examples of common MAT drugs include methadone, Suboxone and Vivitrol.
When providing MAT in-house, addiction treatment centers will be required by federal guidelines to have a medical professional, whether that's a practice nurse, physician assistant, or advanced-practice pharmacist, on staff to dispense medication. Many states require additional credentials or conditions on top of these blanket federal requirements, so check your local regulations to be sure that you're complying with all applicable laws and regulations.
Are Addiction Treatment Centers Who Dispense MAT Considered “Providers” or “Pharmacies” by Express Scripts?
There is no single answer to this question. It depends on how closely you decide to work with Express Scripts at your addiction treatment facility.
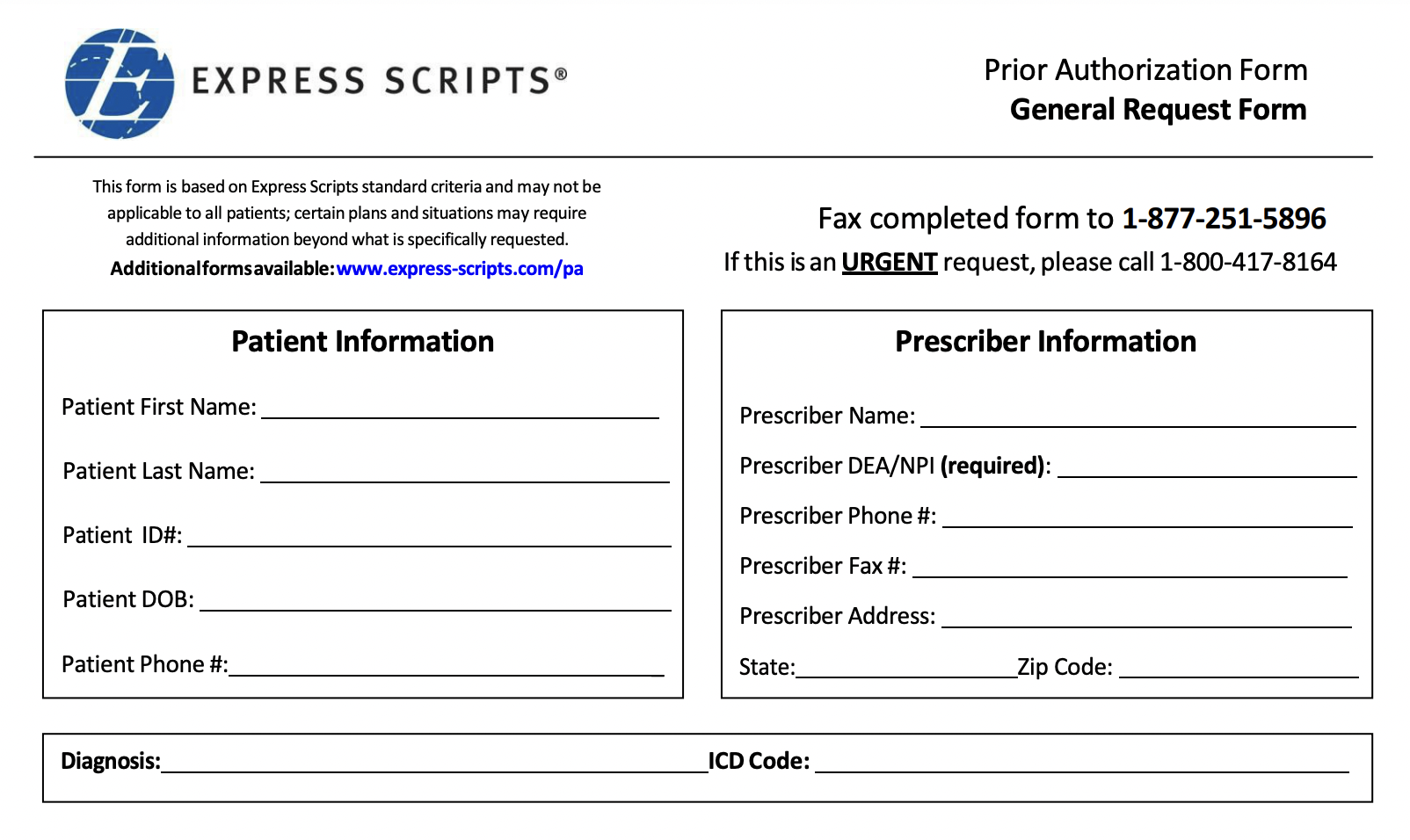
If you want to be treated as an enrolled pharmacy with Express Scripts, you’ll need to complete credentialing and enroll as a participating pharmacy. In order to do that, you can email Express Scripts at NetworkCompliance@express-scripts.com with your pharmacy NCPDP number. Express Scripts urges all would-be participating pharmacies to remember that it can take up to 30 days to actually complete the enrollment process after Express Scripts receives your signed contract and completed application.
If you want to be treated as a provider, you do not need to complete an enrollment process. However, you will need to decide how you want to submit Prior Authorization requests.
What Addiction Treatment Medications Does Express Scripts Cover?
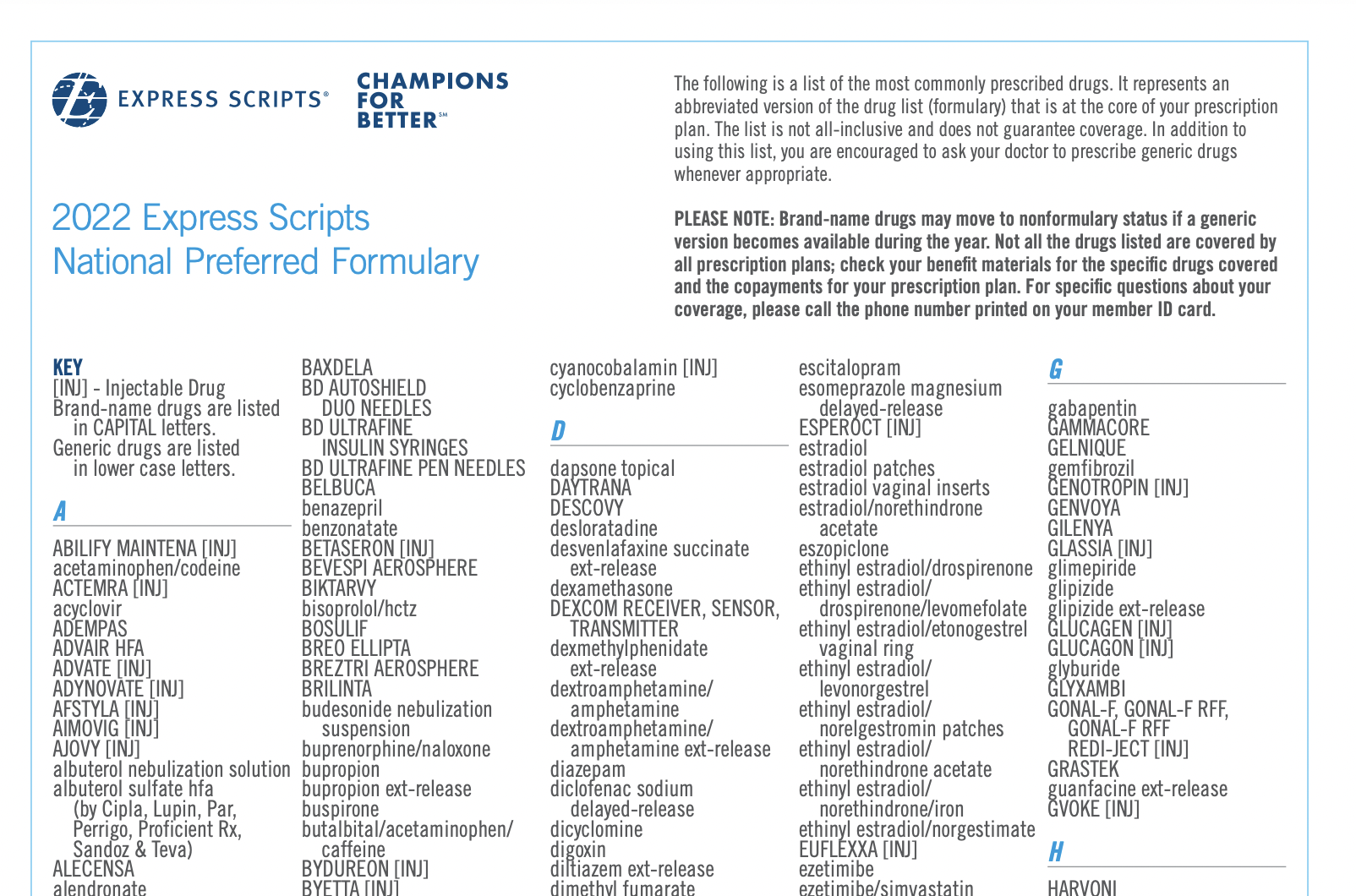
Unlike its leading competitor, CVS Health, Express Scripts covers both methadone and buprenorphine in its formulary. (FYI - A “formulary” is just the technical term for a list of medications that a pharmacy benefit company covers.) Generally speaking, members can access both types of medications, although there are restrictions on certain specifics. For example, certain sublingual film versions of the drugs aren’t covered and name-brand Suboxone isn't covered, while the FDA-approved generic version of buprenorphine is covered by Express Scripts.
When Does Express Scripts Require Prior Authorizations for Addiction Treatment Centers?
Express Scripts requires prior authorizations for many medications, including some medications associated with addiction treatment.
Specifically, Express Scripts requires prior authorization for buprenorphine.
However, Express Scripts does NOT require prior authorization for methadone.
Many psychiatric medications, including many antipsychotics and antidepressants, do require prior authorization with Express Scripts. At addiction treatment centers, it’s not uncommon for dual diagnosis patients to be prescribed medications such as these, as well.
How Do I Complete a Prior Authorization with Express Scripts for my Addiction Treatment Centers’ MAT Medications?
Fortunately, Express Scripts offers providers many options for completing prior authorizations.
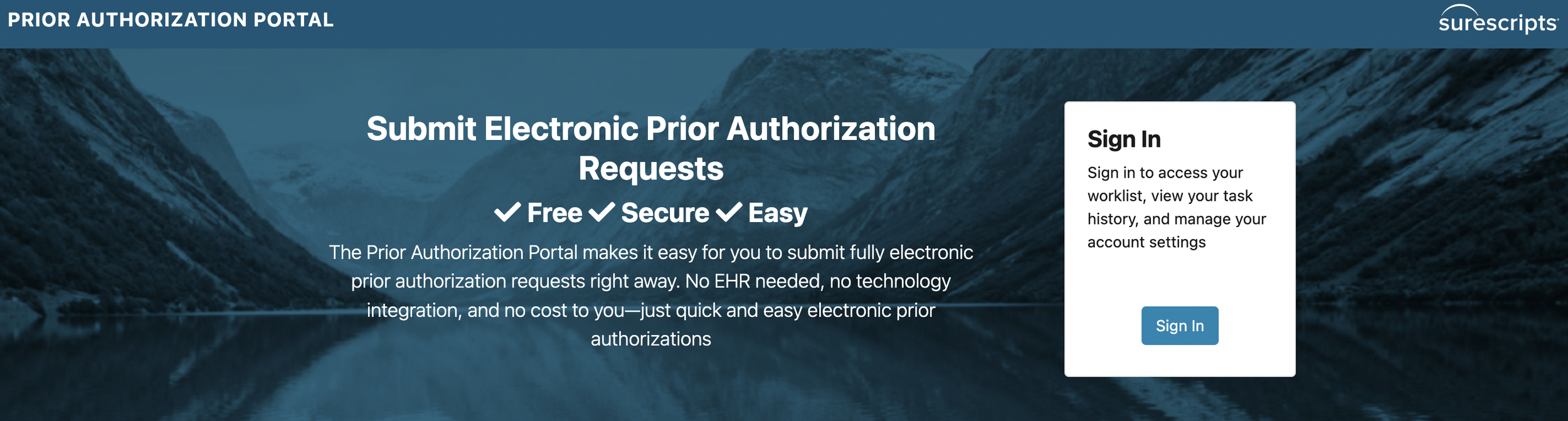
You may:
-Use an EHR with built-in ePA capabilities
-Use one of several ePA provider portals online that works with Express Scripts (such as Surescripts, covermymeds or ExpressPAth)
-Submit traditional paper prior authorization request forms to Express Scripts by fax
Express Scripts states on their website that over 60% of providers submit ePA requests now, but that still leaves 40% of billing departments opting for paper versions. Whatever you choose, Express Scripts will require your NPI number, so have that at the ready.
Trouble with Addiction Treatment Registration for Express Scripts? We Can Help.
BehaveHealth’s Revenue Cycle Management (RCM) service includes soup-to-nuts, hyper-detailed, hands-on attention to every single component of your addiction treatment billing needs. We have strong working relationships with every major insurance company in the United States.
Even better, we’re not health care generalists. We only work for behavioral health providers like you.
Let our team of specialists handle it all:
Verification of Benefits
Utilization Review
Billing and Collections
Patient Responsibility
Denials and Appeals
Get your free trial started today and see why more addiction treatment centers prefer Behave Health.
How to Handle Utilization Reviews with Blue Shield of California for Addiction Treatment
While they’ve done things like make nominal financial contributions to the cause of diversifying the mental healthcare profession, Blue Shield of California is part of a general trend in managed care to minimize costs for insurers by limiting the scope of “medical necessity,” especially when it comes to addiction treatment.