Do you ever feel like you are spending too much of your day weighed down by software snags? Clunky interfaces, slow support, and workarounds for features that never quite deliver pull attention away from what matters most: serving residents and running your operations smoothly. If your team spends more time fixing technical issues than supporting recovery, it’s not just inconvenient. It’s a direct roadblock to growth.
Your software choice can make the difference between the ability to scale and frustrating stagnation. Recovery residence operators need tools built for their real-world challenges.
Why Good Intentions from software Aren’t Enough
Many platforms launch with big promises. They advertise intuitive systems, automated billing, and document management designed to simplify daily work. The reality is often different. Updates cause more problems than they solve, key features require multiple steps to function, and support teams vanish when urgent issues arise. Busy operators are forced to scramble, reverting to paper forms and spreadsheets just to keep things moving.
If this sounds familiar, your software may be standing squarely in the way of your growth.
The Cost of Hidden Inefficiencies
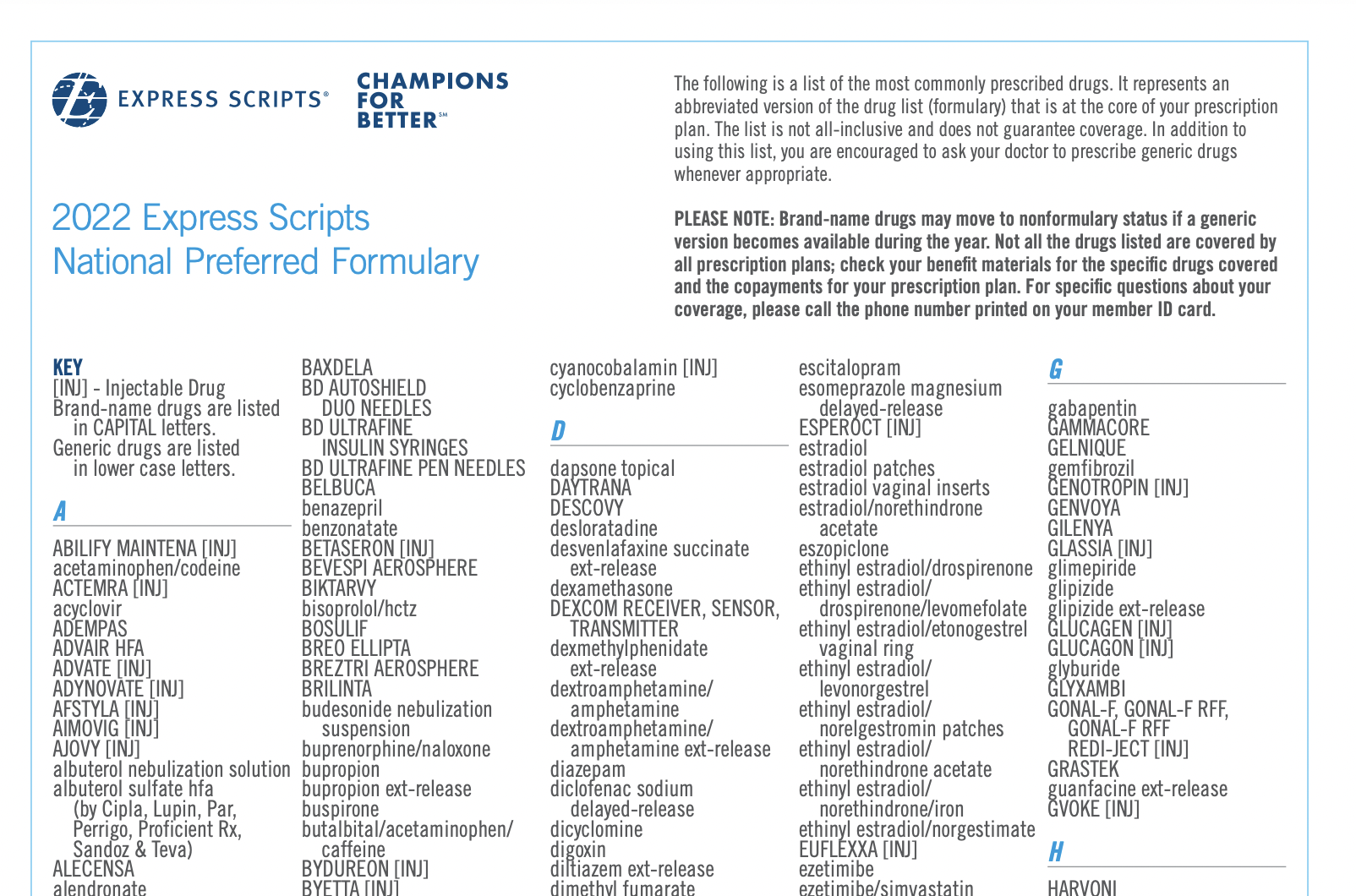
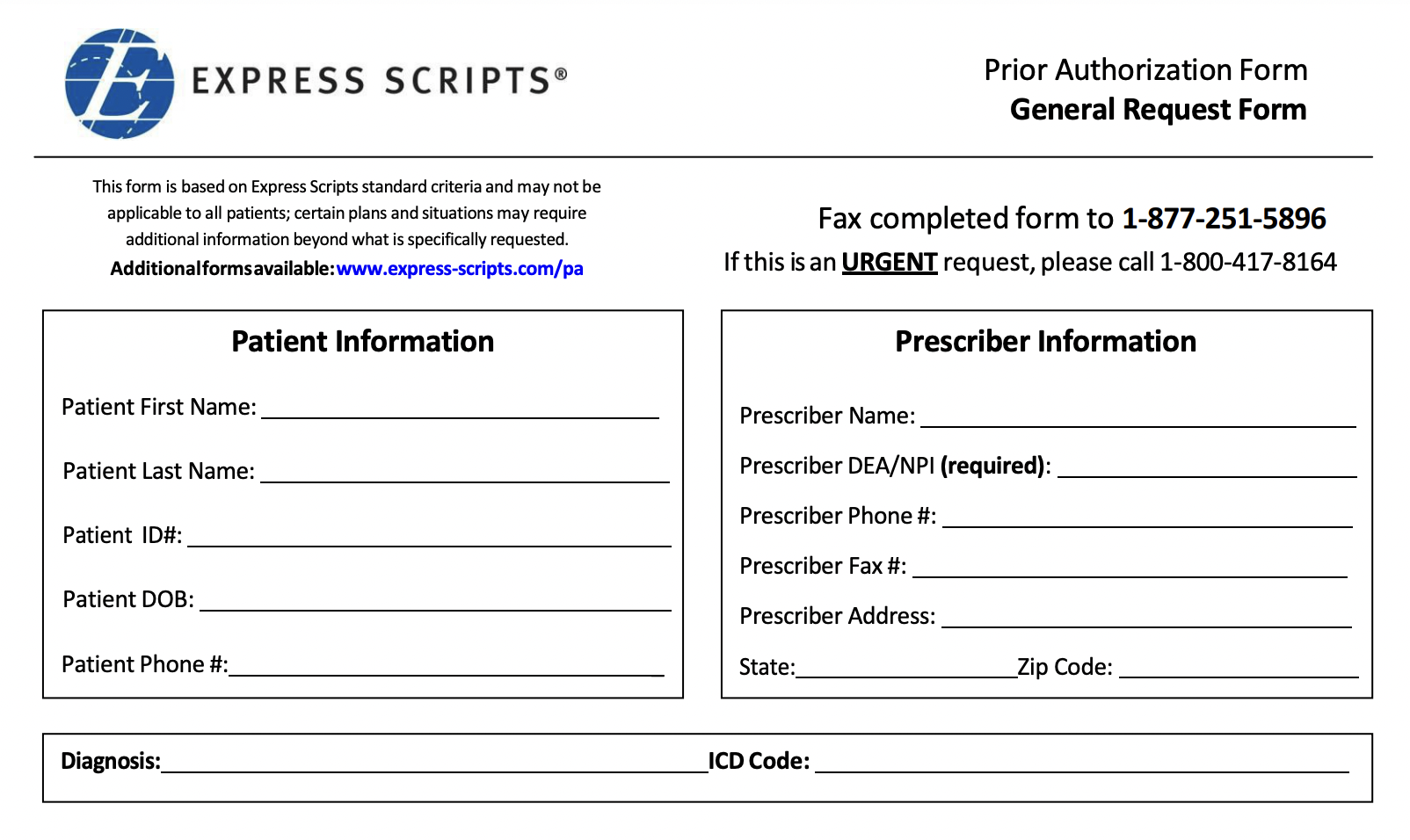
The feedback from recovery residence operators about other recovery residence management software is consistent. Staff cannot complete an intake or application form without glitches or manual uploads. They struggle with an inability to capture automatic payments, partial payments, or back dated payments. There are no permission-based staff roles. There is no way to turn visibility of certain features on or off for streamlined workflows. The list goes on. To top it off, when they reach out for help, customer support takes days or weeks to reply, if they reply at all.
These inefficiencies carry real costs. Burnt out staff. Missed resident appointments. Double data entry. Staff hours wasted chasing fixes. Surprise price hikes. What might seem like isolated frustrations can stall your ability to expand or improve services for residents.
What Growth-Focused Recovery Residence Operators Really Need
Recovery residence operations require more than ideas on paper. They need solutions designed by people who understand their day-to-day realities and test every feature in genuine operational workflows.
Speed and quality of support: Real people answer calls in minutes so your team isn’t left waiting when issues threaten resident care. Weekly office hours available to talk face to face with someone.
Simplicity: Dashboards and portals that work every time, without confusing steps or resorting to backups on paper.
Customizable: The ability to turn the visibility of features on or off based on your unique workflows.
Flexible payments: Integrated ACH, credit card, partial payment ability, and balance tracking systems to keep finances clean, auditable, and hassle-free.
Staff permissions: Role-based permissions that let you manage roles, restrict access, and empower every team member securely.
Transparent pricing: No surprise jumps, grandfathered terms, or hidden fees—a predictable, honest partnership from day one.
Behave Health: Modern Tools for Recovery Residence Growth
Behave Health’s all-in-one software was built specifically for recovery residences that want to grow without losing operational control or service quality. Our platform offers intuitive navigation, reliable performance, and industry-leading support.
Operators switching to Behave Health report faster workflows, less paperwork, and more time to focus on residents. Every feature is designed with operators in mind. Your technology should work as hard as you do.
“Exactly what we were looking for.
Excellent! The customer service from Behave Health is the most hands on and responsive that I have received in a very long time. The features and capabilities were the best part of this software.”
Make the Switch
If your current system leaves you with clunky workarounds, unreliable support, and unpredictable bills, it’s time to change. Your growth should never be held back by yesterday’s software.
Ready to upgrade to a solution that puts your team and residents first?
Book a free demo with Behave Health today. Reclaim your productivity, clarity, and peace of mind.