DISCLAIMER: This content is for general information only and not medical, clinical, legal, financial, compliance, or regulatory advice. No professional relationship is formed. Consult qualified professionals before acting. We disclaim liability for reliance on this content. Use of this page constitutes acceptance of these terms.
In this article we will discuss:
Why Progress Notes Matter in Addiction Treatment
Progress notes are the clinical backbone of substance use disorder (SUD) treatment documentation. For addiction counselors, therapists, and treatment center staff, these notes serve multiple critical functions: they track a client's recovery journey, demonstrate medical necessity for continued treatment, ensure compliance with both HIPAA and 42 CFR Part 2 regulations, and provide legal protection for both clients and clinicians.
In addiction treatment settings, high-quality progress notes ensure continuity of care when clients transition between levels of care or when different team members are involved. They also serve as legal documents that can protect your practice by evidencing the services provided and your clinical decision-making process.
However, documentation in SUD treatment comes with unique challenges. Counselors must balance clinical detail with brevity, maintain person-first language that reduces stigma around addiction, comply with stricter privacy regulations under 42 CFR Part 2, and clearly demonstrate how each session addresses treatment plan goals aligned with ASAM criteria.
This comprehensive guide will help you master SUD progress note writing by covering essential formats (SOAP, DAP, BIRP), compliance with federal regulations, best practices for documenting relapse and recovery, common pitfalls to avoid, and strategies for using EHR technology to streamline your workflow.
What Are SUD Progress Notes?
SUD progress notes are clinical records that addiction professionals complete after each treatment session or significant client encounter. They document the client's status, progress toward recovery goals, and response to interventions. Essential components include.
Client presentation and engagement: Observations of sobriety status, withdrawal symptoms, mood, appearance, and participation level
Subjective reports: The client's own description of their recovery status, cravings, triggers, or challenges since the last session
Interventions used: Specific techniques employed (motivational interviewing, relapse prevention strategies, cognitive-behavioral techniques, 12-step facilitation)
Client response: How the client engaged with interventions and any observable changes during the session
Assessment: Clinical interpretation of progress, relapse risk, and current needs relative to ASAM dimensions
Plan: Next steps including homework, recovery support activities, referrals, or adjustments to the treatment plan
Progress notes serve critical purposes in addiction treatment: they track recovery progress over time, coordinate care across treatment team members and external providers, justify medical necessity for insurance reimbursement, support ASAM level-of-care determinations, and provide legal documentation of treatment services.
Progress Notes vs. SUD Counseling Notes
A critical distinction for SUD professionals is the difference between progress notes and SUD counseling notes (also called process notes). Under the revised 42 CFR Part 2 regulations, SUD counseling notes receive special privacy protections similar to HIPAA's psychotherapy notes.
SUD counseling notes are personal notes that an SUD or mental health professional voluntarily maintains separate from the client's official treatment record. These notes contain the counselor's private analysis of counseling session conversations and clinical impressions that may not be appropriate for the medical record.
Progress notes, by contrast, are the required documentation of treatment sessions that become part of the official clinical record. They include information such as:
Session dates and duration
Services provided and interventions used
Assessment of client's SUD status and progress
Treatment plan updates
Medication prescribed or monitored
Summary of diagnosis and functional status
Why this matters: Progress notes are generally accessible for treatment, payment, and healthcare operations under standard consent, while SUD counseling notes require specific separate consent from the client and cannot be disclosed based on broad treatment consent. Insurance companies and courts can request progress notes, but they cannot compel disclosure of SUD counseling notes.
This guide focuses on progress notes—the formal record of each session that documents clinically relevant information and treatment provided.
Common Progress Note Formats for addiction Treatment
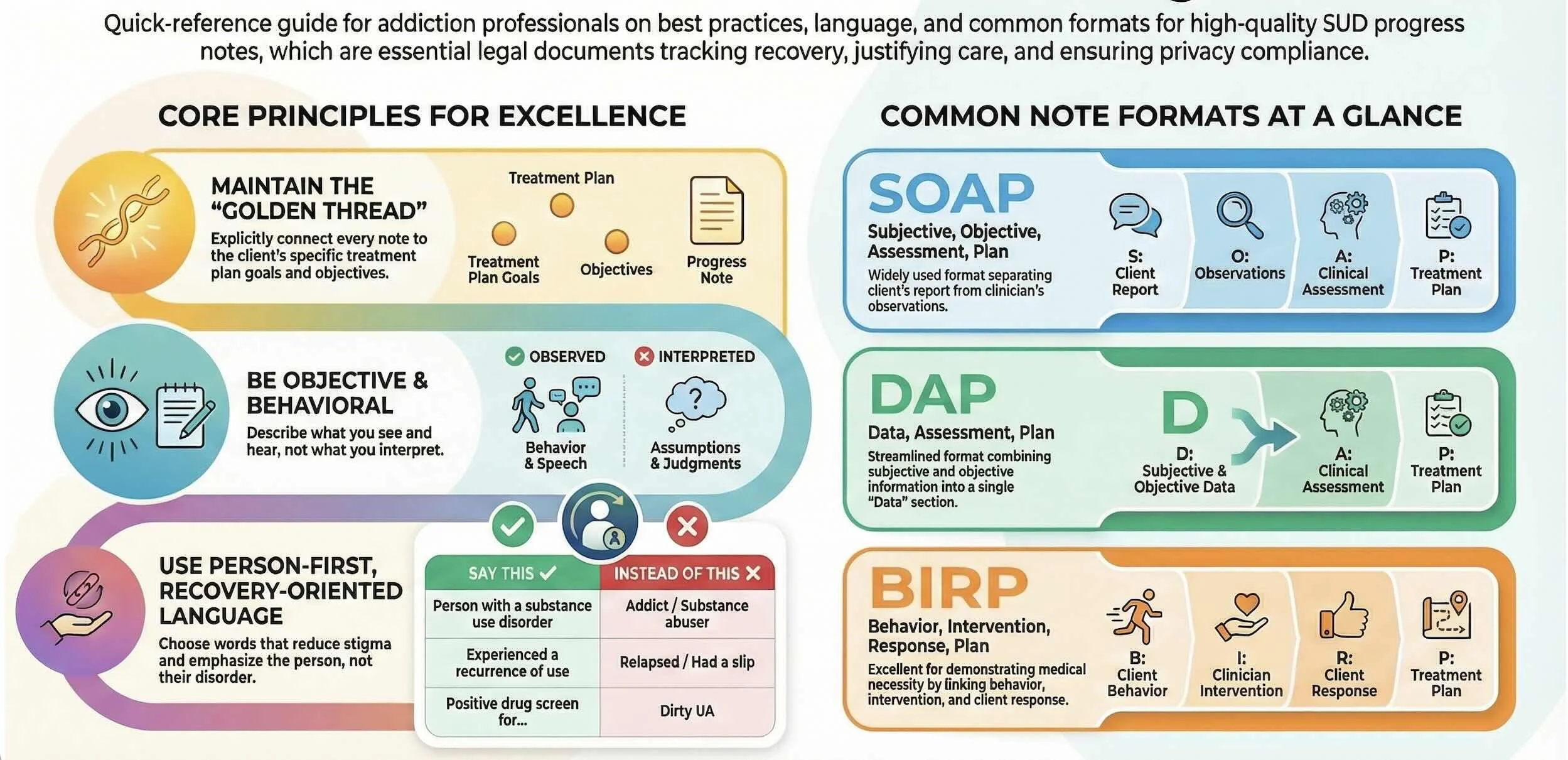
SOAP Notes
SOAP (Subjective, Objective, Assessment, Plan) is widely used across addiction treatment settings:
Subjective (S): Client's self-reported status including sobriety days, cravings, triggers encountered, support group attendance, and emotional state. Example: "Client reports 14 consecutive days of sobriety. States cravings have decreased from '8/10 to 4/10' this week. Attended four AA meetings and connected with sponsor daily."
Objective (O): Counselor's observations including appearance, affect, drug screening results, withdrawal symptoms, and behavioral observations. Example: "Client appeared well-groomed with improved eye contact. Speech clear and coherent. UDS negative for all substances. No observable withdrawal symptoms."
Assessment (A): Clinical analysis of the client's current status, progress toward goals, and relapse risk. Example: "Client demonstrates continued progress in early recovery with improved coping skills and strong engagement with recovery supports. Relapse risk assessed as moderate due to upcoming social triggers (family gathering). Depression symptoms remain mild."
Plan (P): Treatment interventions and next steps. Example: "Practiced refusal skills via role-play for upcoming family event. Client will complete trigger log daily and attend minimum of three support groups this week. Continue weekly individual counseling focusing on relapse prevention. Next session will review trigger log and refine safety plan."
DAP Notes
DAP (Data, Assessment, Plan) combines subjective and objective information into a single "Data" section:
Data (D): "Client reports 7 days sober and attending 3 support meetings weekly. Expressed anxiety about job interview where previous coworkers used substances together. Noted client was fidgeting and reported sleep difficulties (5 hours per night). UDS results pending."
Assessment (A): "Client shows good insight into relapse triggers related to work environment. Anxiety symptoms remain elevated, likely contributing to sleep difficulties and increased relapse risk. Client is utilizing sponsor support and attending meetings consistently, which are protective factors."
Plan (P): "Continue weekly individual counseling with focus on managing anxiety and workplace triggers. Client will practice grounding techniques twice daily and document in recovery journal. Referred to psychiatry for anxiety evaluation. Will review UDS results and adjust treatment plan if needed next session."
BIRP Notes
BIRP (Behavior, Intervention, Response, Plan) is particularly effective for demonstrating medical necessity in addiction treatment:
Behavior (B): "Client arrived on time stating, 'I had a slip this weekend—used on Saturday night.' Appeared tearful and ashamed. Reported three days without substance use since then. Attended one AA meeting post-use."
Intervention (I): "Counselor used motivational interviewing to explore circumstances of use and identify triggers. Normalized relapse as part of recovery process while reinforcing client's return to sobriety. Reviewed and updated relapse prevention plan, identifying warning signs client missed (isolation, skipping meals, overconfidence). Practiced urge surfing technique."
Response (R): "Client initially defensive, stating 'I knew I'd fail.' After exploration, client identified key trigger (relationship conflict) and recognized warning signs. Engaged well in updating safety plan and practicing coping skill. By session end, client stated, 'I can learn from this' and committed to increased accountability."
Plan (P): "Client will contact sponsor daily and increase support meetings to one per day for next week. Will complete daily check-ins with counselor via phone. Schedule family session to address relationship stressors. Continue individual counseling twice weekly for next two weeks, then reassess frequency."
BIRP format clearly links the client's presentation to interventions and outcomes, which is essential for justifying continued treatment to payers and demonstrating progress toward treatment goals.
Best Practices for SUD Progress Notes
Document Timely and Accurately
Complete notes within 24-48 hours of the session while details are fresh. In addiction treatment, timely documentation is especially critical when clients are in early recovery or at elevated relapse risk.
Connect Every Note to the Treatment Plan
Each progress note should explicitly link to treatment plan goals. If the treatment plan goal is "Client will maintain sobriety from alcohol," your note should reference sobriety status and interventions addressing this goal. This creates a clear "golden thread" connecting assessment, treatment planning, progress notes, and outcomes.
Use Person-First, Recovery-Oriented Language
Always use person-first language that emphasizes the individual, not their addiction:
Say: "Person with substance use disorder" Not: "Addict" or "Substance abuser"
Say: "Client experienced recurrence of use" Not: "Client relapsed again"
Say: "Person in recovery" Not: "Recovering addict"
Say: "Client has not taken medications as prescribed" Not: "Client is non-compliant"
Say: "Positive drug screen for methamphetamine" Not: "Dirty UA"
Say: "Client used substances" Not: "Client abused drugs"
Avoid stigmatizing terms like "clean" (implies "dirty" when using), "habit," "junkie," or "drunk." These terms reinforce shame and can damage therapeutic relationships.
Document Both Strengths and Challenges
Balanced documentation reflects the full clinical picture. Include:
Protective factors: Support system, employment, housing stability, motivation
Progress: Days sober, skills learned, insights gained, improved functioning
Challenges: Triggers encountered, cravings, barriers to treatment, relapse risk factors
Engagement: Attendance, participation quality, homework completion
Example: "Client maintains 30 days sobriety (strength) and reports strong family support (protective factor). However, client missed two group sessions this week (challenge) and reports increased cravings related to work stress (risk factor)."
Clearly Document Interventions and Responses
Every SUD progress note should answer: What specific intervention did I use? and How did the client respond?
Examples of SUD interventions to document:
Motivational interviewing techniques (open-ended questions, reflective listening, decisional balance)
Cognitive-behavioral strategies (thought records, cognitive restructuring, behavioral experiments)
Relapse prevention (trigger identification, coping skills training, safety planning)
12-step facilitation
Contingency management
Mindfulness/meditation exercises
Family systems work
Psychoeducation about addiction neurobiology
Document the response: "Client initially ambivalent about attending AA, stating 'I don't think that's for me.' After exploring concerns using MI, client agreed to attend one meeting before next session 'just to see.' Client appeared more open by session end."
Address Relapse Risk and Safety Planning
Regularly assess and document relapse risk factors and protective factors. Include:
Current triggers and high-risk situations identified
Warning signs of potential relapse
Coping strategies available
Support system strength
Safety plan elements
Example: "Relapse risk assessed as moderate-high due to upcoming holiday (high-risk situation) and recent job loss (stressor). Protective factors include stable housing, engaged sponsor, and 90 days sobriety. Safety plan reviewed and updated with client agreeing to daily sponsor contact and avoiding family gathering where alcohol will be present."
Comply with 42 CFR Part 2 Privacy Regulations
SUD treatment records have stricter confidentiality protections than general medical records. Key considerations:
Obtain proper consent before disclosing any SUD treatment information, even to other healthcare providers
Include consent scope with any disclosure of SUD records—either attach a copy of consent or clearly explain its scope
Minimize information disclosed: Only share what is necessary for the stated purpose
Maintain SUD counseling notes separately if you keep them, ensuring they are only accessible to the treating clinician
Never disclose that someone is or has been in SUD treatment without proper consent
Document ASAM Dimensions When Relevant
Reference ASAM's six dimensions when documenting assessment and progress, particularly for level-of-care decisions:
Acute intoxication and/or withdrawal potential
Biomedical conditions and complications
Emotional, behavioral, or cognitive conditions
Readiness to change
Relapse, continued use, or continued problem potential
Recovery/living environment
Example: "Client's withdrawal symptoms have resolved (Dimension 1). Hypertension stable with medication (Dimension 2). Depression improving with increased activities (Dimension 3). Client demonstrates action stage of change with strong commitment to recovery (Dimension 4). Moderate relapse risk due to environmental triggers (Dimension 5). Living environment supportive with sober roommate (Dimension 6). Client appropriate for intensive outpatient level of care."
Be Objective and Behavioral
Describe observable behaviors rather than interpretations:
Objective: "Client's speech was slurred, gait unsteady, and strong odor of alcohol detected"
Subjective: "Client appeared drunk"
Objective: "Client stated 'I don't have a problem, everyone drinks like I do'"
Subjective: "Client is in denial"
Keep Notes Concise Yet Comprehensive
Most outpatient SUD progress notes are 150-350 words—enough to cover critical elements without becoming a transcript. Focus on what is clinically relevant to treatment goals and medical necessity.
Common Documentation Mistakes in SUD Treatment
Failing to Document Recurrence of Use Appropriately
When a client returns to substance use, document thoroughly and non-judgmentally:
Substances used, amount, duration
Circumstances and triggers
Client's response and current status
Interventions provided
Updated safety plan
Any changes to treatment plan or level of care
Never minimize or omit documentation of substance use—this creates liability and continuity of care issues.
Not Demonstrating Medical Necessity
Insurance requires clear evidence that treatment is medically necessary. Each note should show:
Why this level of care is appropriate
How the session addressed treatment needs
That less intensive treatment would be insufficient
Progress (or clinical rationale for continued treatment if progress is limited)
Using Stigmatizing Language
Avoid terms like "addict," "alcoholic," "clean/dirty," "substance abuser," or "drug seeker". These terms can:
Damage therapeutic relationships if clients read their records
Bias other providers who read the notes
Create legal vulnerabilities
Violate person-first language standards
Inadequate Safety and Risk Documentation
Trigger Warning: Substance use, overdose, and suicide mentioned.
Always document:
Overdose history and current risk
Suicidal ideation, especially during withdrawal or early recovery
Access to substances or means of self-harm
Safety planning and risk mitigation strategies
Consultations with supervisors or medical providers regarding risk
Example: "Client expressed passive suicidal ideation stating 'Sometimes I think everyone would be better off without me' but denies current plan or intent. Reports history of overdose (2023) during active use. Currently 45 days sober with no current substance access. Completed safety plan including crisis hotline number and agreement to contact sponsor if urges intensify. Will monitor closely in next session. Consulted with clinical supervisor (J. Smith, LCSW) who recommended continued weekly individual counseling."
Copy-Pasting Previous Notes
Each session is unique—never copy/paste entire notes from previous sessions. This can lead to:
Inaccurate sobriety dates
Outdated risk assessments
Billing fraud allegations
Failure to capture actual session content
Missing the Connection to SMART Goals
Treatment plans should include SMART goals (Specific, Measurable, Achievable, Relevant, Time-bound), and progress notes should track progress toward these goals:
Treatment Plan Goal: "Client will maintain abstinence from alcohol for 90 consecutive days by June 1, 2025"
Progress Note: "Client reports 47 days of continuous sobriety (progress toward 90-day goal). Client identified and successfully navigated two high-risk situations this week using relapse prevention skills practiced in previous sessions."
Documenting Different SUD Treatment Modalities
Individual Counseling
Focus on the individual client's recovery journey, including specific interventions, client responses, and progress toward personalized goals. Document treatment modality used (MI, CBT, relapse prevention) and specific techniques applied.
Group Therapy
Write a separate note for each group member—never one combined note. For each client:
Describe the group topic/activity
Document that specific client's participation level and contributions
Note any peer interactions or support that client provided/received
Avoid using full names of other group members
Example: "Group topic: Managing triggers and cravings. Client actively participated by sharing personal experience with workplace triggers and how he successfully used urge surfing technique this week. Provided supportive feedback to another member struggling with family conflict. Client appeared engaged throughout and stated, 'Hearing others' stories helps me feel less alone.' Plan: Continue weekly process group."
Family Sessions
Document who was present and how the session relates to the client's treatment goals:
Example: "Family session with client and spouse present. Addressed communication patterns around client's recovery and spouse's concerns about trust rebuilding. Client practiced 'I' statements when discussing need for recovery meeting attendance. Spouse expressed willingness to attend Al-Anon. Both agreed to weekly family check-ins. Client reported session was 'helpful' and expressed commitment to transparency about recovery activities."
Medication-Assisted Treatment (MAT)
When documenting MAT services:
Note medication name, dosage, and administration
Document side effects or concerns
Address adherence and effectiveness
Link to overall treatment plan and recovery goals
Example: "Client received buprenorphine/naloxone 16mg/4mg sublingual under observation. Reports medication 'helps with cravings significantly.' Denies side effects. Last use of illicit opioids: 62 days ago. UDS negative for opioids, positive for prescribed buprenorphine. Counseling session focused on continued recovery support engagement and return-to-work planning. Client maintaining stability on current MAT regimen."
Telehealth Sessions
Clearly indicate when services are provided via telehealth and document:
Platform used and technology functioning
Client's location and privacy
Any limitations of virtual format
Clinical content as you would for in-person sessions
Example: "Telehealth session conducted via BehaveHealth secure platform. Client in private location at home. No technology difficulties. Conducted weekly individual counseling using CBT for co-occurring depression and alcohol use disorder..."
Leveraging EHR Technology for Efficient SUD Documentation
Modern EHR systems designed for behavioral health can dramatically improve documentation efficiency while maintaining compliance:
Customizable Templates
Use SUD-specific templates that prompt you to include all required elements:
Sobriety status and date of last use
UDS results
ASAM dimension updates
Treatment plan goal progress
Relapse risk assessment
Safety planning elements
Auto-populated Fields
Let technology handle administrative details:
Client demographics
Diagnosis codes
CPT codes for billing
Session dates and duration
Provider signatures and credentials
Integrated Treatment Planning
Connect progress notes directly to treatment plans within your EHR so you can easily reference goals and track progress without switching screens.
42 CFR Part 2 Compliance Features
Choose an EHR that supports:
Proper consent management for SUD records
Separation of SUD counseling notes from progress notes
Disclosure tracking with consent attachment
Role-based access controls
Voice-to-Text and AI Assistance
Some modern EHRs offer voice dictation or AI-powered documentation assistance to speed up note-writing while maintaining clinical quality. Always review and edit AI-generated content for accuracy.
Conclusion: Excellence in SUD Documentation
Mastering progress note documentation is essential for providing high-quality addiction treatment. Well-written notes support continuity of care, demonstrate medical necessity, ensure regulatory compliance, and protect both clients and clinicians.
By implementing the best practices outlined in this guide—using person-first language, connecting notes to treatment goals, documenting both progress and challenges, maintaining appropriate privacy protections, and leveraging EHR technology—you can create documentation that is both clinically valuable and efficiently completed.
Remember: Your progress notes tell the story of your client's recovery journey. Make that story clear, compassionate, and clinically sound.
Ready to streamline your SUD treatment documentation?
Learn how Behave Health's EHR can help your addiction treatment center maintain compliant, efficient clinical documentation while giving you more time to focus on client care.