Does your addiction treatment center do a lot of billing with Blue Cross Blue Shield of Minnesota? If the answer is yes, then that wouldn’t be a huge surprise. BCBSM is the state’s largest provider of insurance, with over one in three Minnesotans carrying a plan. The non-profit affiliate is also one of the earliest BCBS affiliates in the country, having been in operation in the area since the 1930’s.
BCBSM boasts a net operating income of $128 million and banks over $13 billion in revenue per year. With recent CEO turnover and a declining membership base, the future of Blue Cross Blue Shield in Minnesota is slightly cloudy but, nonetheless, the payer still sees a lot of addiction treatment activity among its diverse membership base.
Can I Use a Billing Claims Address for Addiction Treatment Billing with Blue Cross Blue Shield of Minnesota?
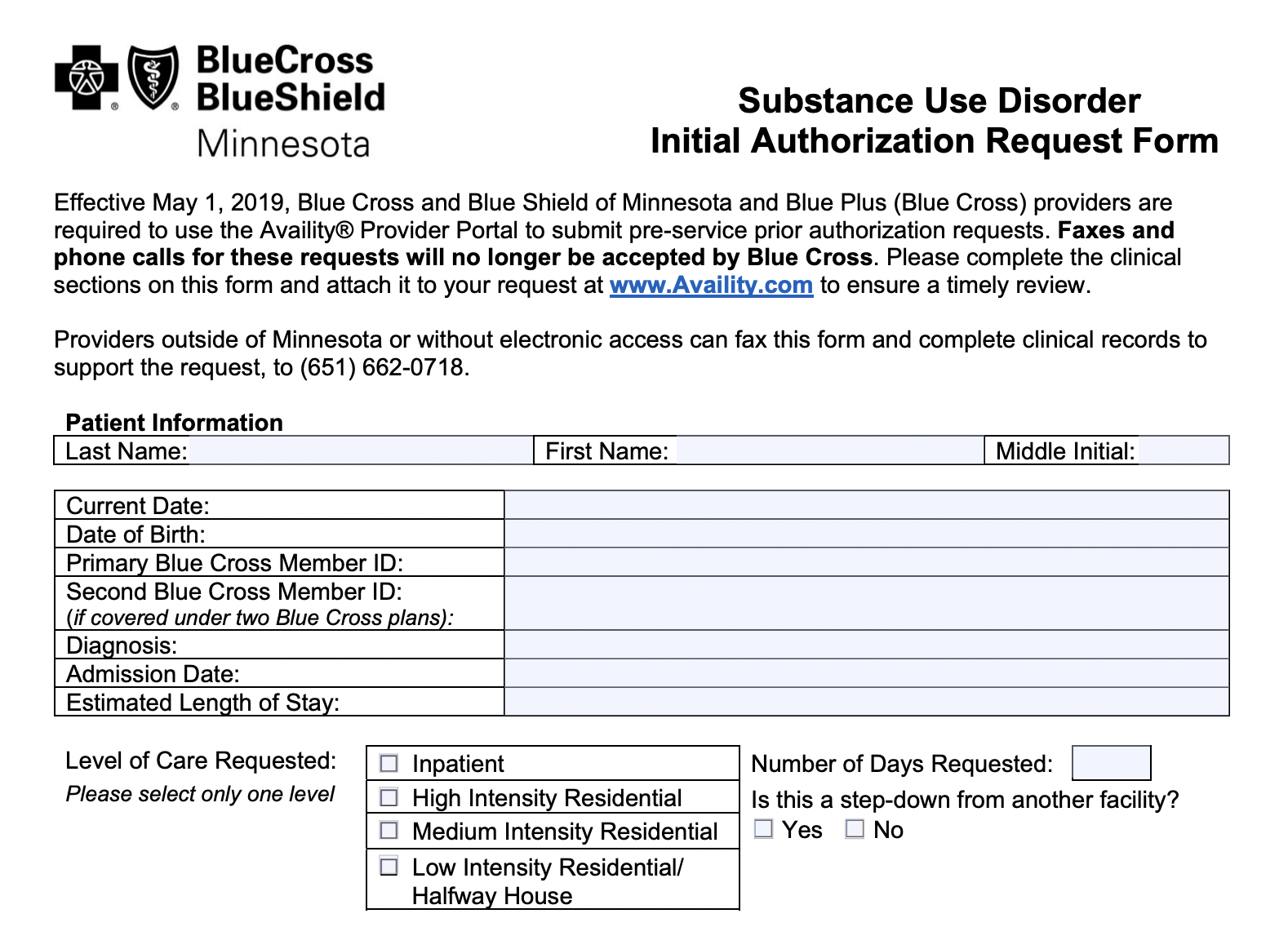
There are physical addresses to which you can send addiction treatment billing claims to Blue Cross Blue Shield of Minnesota. That said, there are many forms - especially many addiction treatment specific forms - that you should NOT attempt to mail to BCBSM. Blue Cross Blue Shield of Minnesota is still accepting paper billing claims from addiction treatment centers but they are NOT accepting all utilization management forms by mail.
You can access many clinical forms for behavioral health on the BCBSM website, but it’s important to know that many of these forms cannot actually be submitted outside of the Availity system.
If you’re sure the form you want to send can be submitted via mail, then the physical billing claims address you’ll want to use is:
Blue Cross and Blue Shield of Minnesota
Document Processing Center
P.O. Box 982805
El Paso, TX 79998-2805
If You’re Seeking an Adjustment or an Appeal as a Provider, You’ll Use a Different Address. That Address is:
Blue Cross and Blue Shield of Minnesota
Document Processing Center
P.O. Box 982800
El Paso, TX 79998-2800
Not sure if you can submit the form via regular mail? Read on to learn more about what can and cannot be sent via physical mail to BCBSM for addiction treatment billing claims.
Blue Cross Blue Shield of Minnesota Wants All Providers - Including Addiction Treatment Providers - to Submit Paperwork Through Availity
Blue Cross Blue Shield of Minnesota has joined many other BCBS affiliates in adopting Availity - an increasingly commonplace EDI Clearinghouse - to take care of such paperwork as prior authorization requests.
In fact, as of 2019, BCBSM stopped accepting any form of prior authorization request - including those that are faxed or phoned in - in favor of an all-Availity system. All prior authorization requests now must be submitted through the Availity Provider Portal. You can log into the system here if you already have established an account.
Familiarize Yourself With Blue Cross Blue Shield of Minnesota’s Clinical Criteria Guidelines for Behavioral Health Before You Start Looking for the Billing Claims Address
It’s always worthwhile to familiarize yourself with the clinical criteria guidelines that BCBSM uses to make coverage and medical necessity determinations for addiction treatment and behavioral healthcare prior authorization requests and claims submissions.
The clinical guidelines tell you what specific benchmarks and clinical criteria must be met in order to establish coverage for any given service.
Unfortunately, BCBSM draws from several different sets of criteria and guidelines and synthesizes that information in-house, using their Blue Cross Medical and Behavioral Health Policy Committee, making a determination more subjective than objective, The guidelines the committee draws from are: eviCore healthcare clinical guidelines, Federal Employees Programs medical policies rules, and InterQual criteria.
Tired of Searching for the Addiction Treatment Claims Address for BCBSM? We Can Help.
BehaveHealth’s Revenue Cycle Management (RCM) service includes soup-to-nuts, hyper-detailed, hands-on attention to every single component of your addiction treatment billing needs. We have strong working relationships with every major insurance company in the United States.
Even better, we’re not health care generalists. We only work for behavioral health providers like you.
Let our team of specialists handle it all:
Verification of Benefits
Utilization Review
Billing and Collections
Patient Responsibility
Denials and Appeals
Get your free trial started today and see why more addiction treatment centers prefer Behave Health.