BEHAVE HEALTH BLOG
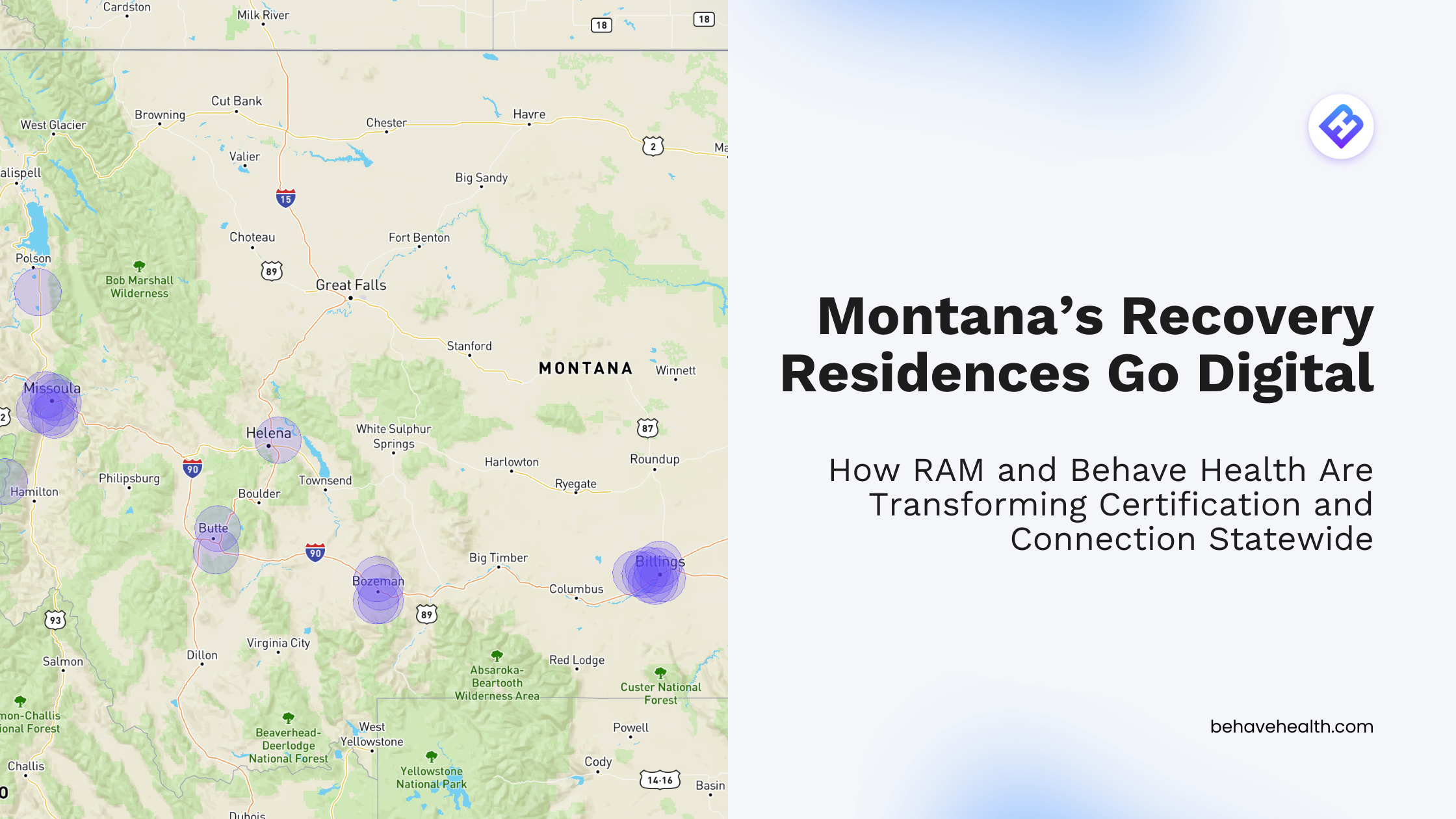
Discover how Montana and Behave Health transformed recovery residence certification and directory management, setting a digital standard for the nation.
The Tennessee Alliance of Recovery Residences (TNARR) has partnered with Behave Health to launch a fully digital recovery residence certification process—streamlining workflows, reducing paperwork, and giving operators real-time tools for bed management, compliance, and outcome tracking. Built on NARR standards and powered by the Behave Affiliate Management Platform (AMP), this innovation transforms certification for Tennessee recovery housing, helping operators save time, improve efficiency, and deliver better resident outcomes.
When Native Solutions set out to launch Mariposa County’s first-ever medication-assisted treatment (MAT) facility, overwhelming licensing hurdles and zero local precedent stood in the way. Partnering with Behave Health Consulting, they turned initial rejection and complex requirements into a groundbreaking success—earning state licensure in record time, bringing vital addiction treatment home to their community, and securing over $1.3 million in funding. Discover how expert regulatory guidance, innovative technology, and local leadership helped redefine rural behavioral healthcare in California.
As M&As have slowed in the addiction treatment space in recent years, many owners, investors, and entrepreneurs in the behavioral health space are accelerating their search for a “sweet spot” between deal flow and business-friendly regulation.
Learn how to leveraged Behave Health before, during, and after the M&A process. Command confidence and consistency throughout your organization as it grows.
There are two new Drug Enforcement Administration (DEA) rules in play this year in 2025. Is your addiction treatment organization ready to adapt?
On March 27th 2025, RFK Jr, head of the Health and Human Services Department in the Trump Administration, announced that SAMHSA will effectively cease to exist.