Healthfirst insurance is a large not-for-profit insurance company based in New York. They provide health insurance to members in New York City, Long Island, Westchester County, Sullivan County, Orange County and Rockland County. One in five New Yorkers have health insurance with Healthfirst and their membership base is highly diverse. They count over $12 billion dollars per year in annual revenue and are known for their public Medicaid and Medicare plans, although they actually offer 5 different types of plans at many different tiers of coverage.
While there have been some complaints about unpaid claims from formerly in-network providers who claim they were unceremoniously booted from Healthfirst’s network, Healthfirst has a generally passable reputation as a payer among addiction treatment providers in the area.
How Does Addiction Treatment Coverage Work With Healthfirst Insurance?
Healthfirst has many different types of plans at many different levels of coverage. They include:
Leaf
Leaf Premiere
Individual Off Exchange Plans
Pro Plans
Pro Plus Plans
While it is difficult to generalize about these plans, as they are all different and they all have many different variations to choose from, all plans cover some aspect of addiction treatment.
In general, out of network providers for addiction treatment and behavioral health care - whether they are offering inpatient or outpatient care - are not covered under Healthfirst. Depending on the plan’s coverage, members can expect to pay between $500 and $1500 copay for inpatient addiction treatment care. Preauthorization is required for all inpatient care, except in the case of emergency. Preauthorization is required for some - but not all - outpatient care, depending on the situation and the level of care.
For more specifics on any one plan’s addiction treatment coverage, you can access all of Healthfirst’s Summary of Benefits here.
How Do Addiction Treatment URs or Utilization Reviews Work With Healthfirst Insurance?
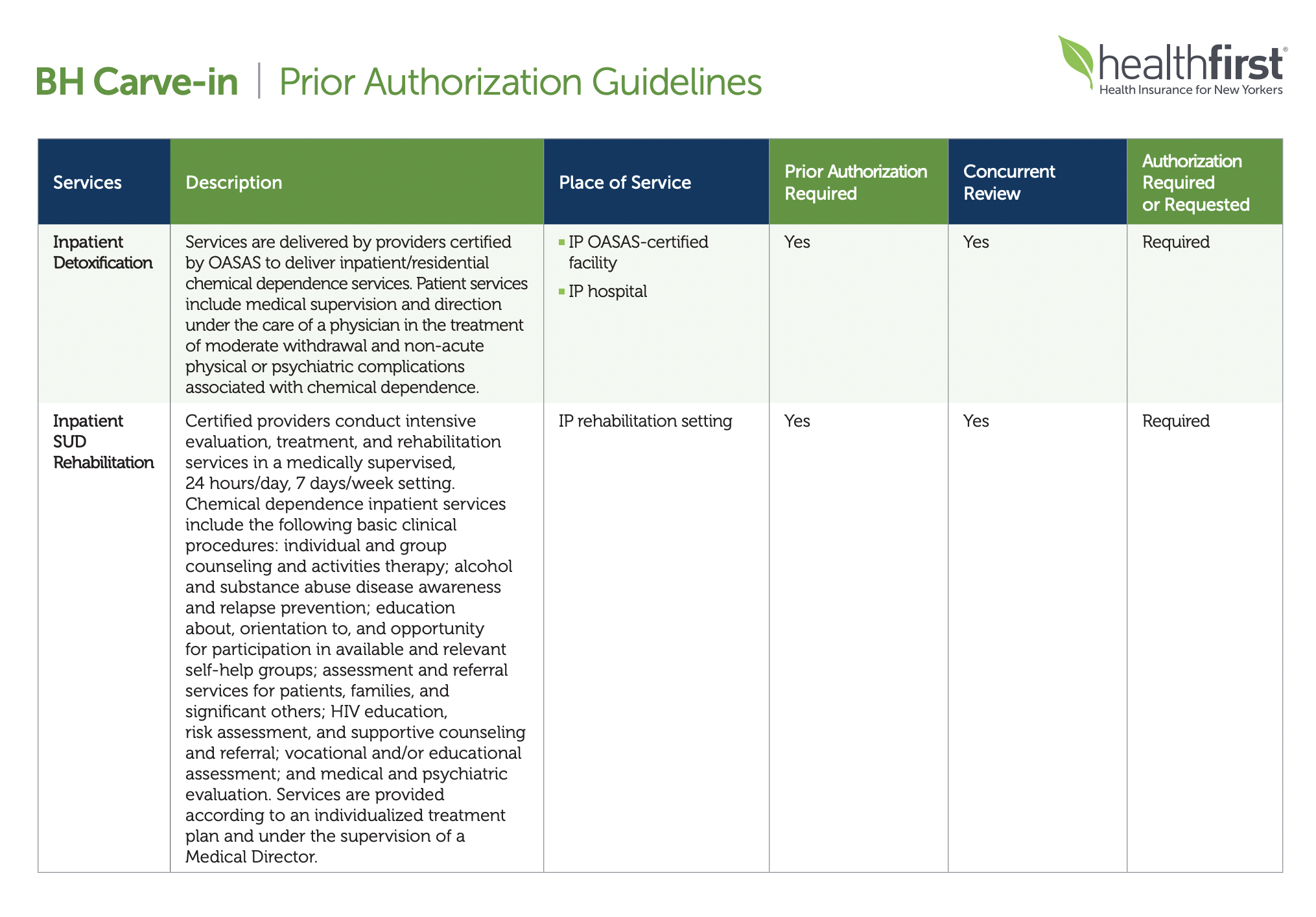
The best document to consult regarding addiction treatment utilization review requirements for Healthfirst Insurance is Healthfirst’s Behavioral Health Carve-In PDF, which lists every imaginable behavioral healthcare treatment and outlines whether prior authorization, concurrent review and/or authorization is required for each.
For example, on page 4, you’ll see that, with Healthfirst Insurance, “Inpatient SUD Rehabilitation” requires prior authorization, concurrent review and authorization.
According to page 58 of Healthfirst’s Provider Manual, providers must connect on the telephone with a Clinical Intake Coordinator at Healthfirst to complete the authorization process. You can reach them at 1-888-394-4327. Providers who are affiliated with ACT, PROS and BH-HCBS can also submit requests for authorization via fax at 1-646-313-4612.
Finally, providers may submit requests for authorization through the provider portal.
What Addiction Treatment Diagnosis Codes Should be Used in Healthfirst Utilization Reviews?
There is no “best” addiction treatment diagnosis code (or ICD-10 code) to use when completing URs or authorizations with Healthfirst. All behavioral health diagnosis codes are subject to more or less the same utilization management decision making criteria at Healthfirst.
In other words, there are no “top 5 addiction treatment diagnosis codes to use” when it comes to completing URs for Healthfirst Insurance. In fairness, that makes the title of this post somewhat of a misnomer.
There are, however, some old standbys that you’ll likely use when completing URs with Healthfirst.
If your patient struggles with alcohol use disorder, you’ll likely use the F10.1 ICD-10 diagnosis code.
If your patient struggles with opioid use disorder, you’ll likely use the F11.1 code.
If your patient struggles with polydrug abuse, you’ll likely use the F19.1 ICD-10 diagnosis code.
If your patient struggles primarily with cocaine abuse, the F14.1 will be your go-to.
If your patient struggles with stimulant abuse primarily, then you’ll use the F15.1 diagnosis code.
Want to Simplify URs or Utilization Reviews with Healthfirst Insurance? We Can Help.
BehaveHealth’s Revenue Cycle Management (RCM) service includes soup-to-nuts, hyper-detailed, hands-on attention to every single component of your addiction treatment billing needs. We have strong working relationships with every major insurance company in the United States.
Even better, we’re not health care generalists. We only work for behavioral health providers like you.
Let our team of specialists handle it all:
Verification of Benefits
Utilization Review
Billing and Collections
Patient Responsibility
Denials and Appeals
Get your free trial started today and see why more addiction treatment centers prefer Behave Health.