Does Molina Healthcare Call it Pre-Certification, Prior Authorization, Preauthorization, Predetermination or Prior Approval?
Whether you call it a pre-certification, a prior authorization, a prior auth, a PA, preauthorization, predetermination or prior approval, the basic concept is the same. Molina happens to prefer the term “prior authorization,” so that’s how we’ll refer to this insurance requirement in this post.
Prior authorizations are required by many health insurance companies for many behavioral healthcare and addiction treatment services, and Molina Healthcare is no exception.
A prior authorization essentially consists of formally asking permission from the health insurance provider to provide a certain service in response to a certain diagnosis code. Upon receiving the request, the insurance provider will determine if the service is medically necessary and if it is covered by the member’s plan.
After the review process, Molina will either issue an authorization or a denial. Members may appeal the denial, if necessary.
Under What Circumstances does Molina Healthcare Require Addiction Treatment Centers to Obtain Prior Authorization or Precertification?
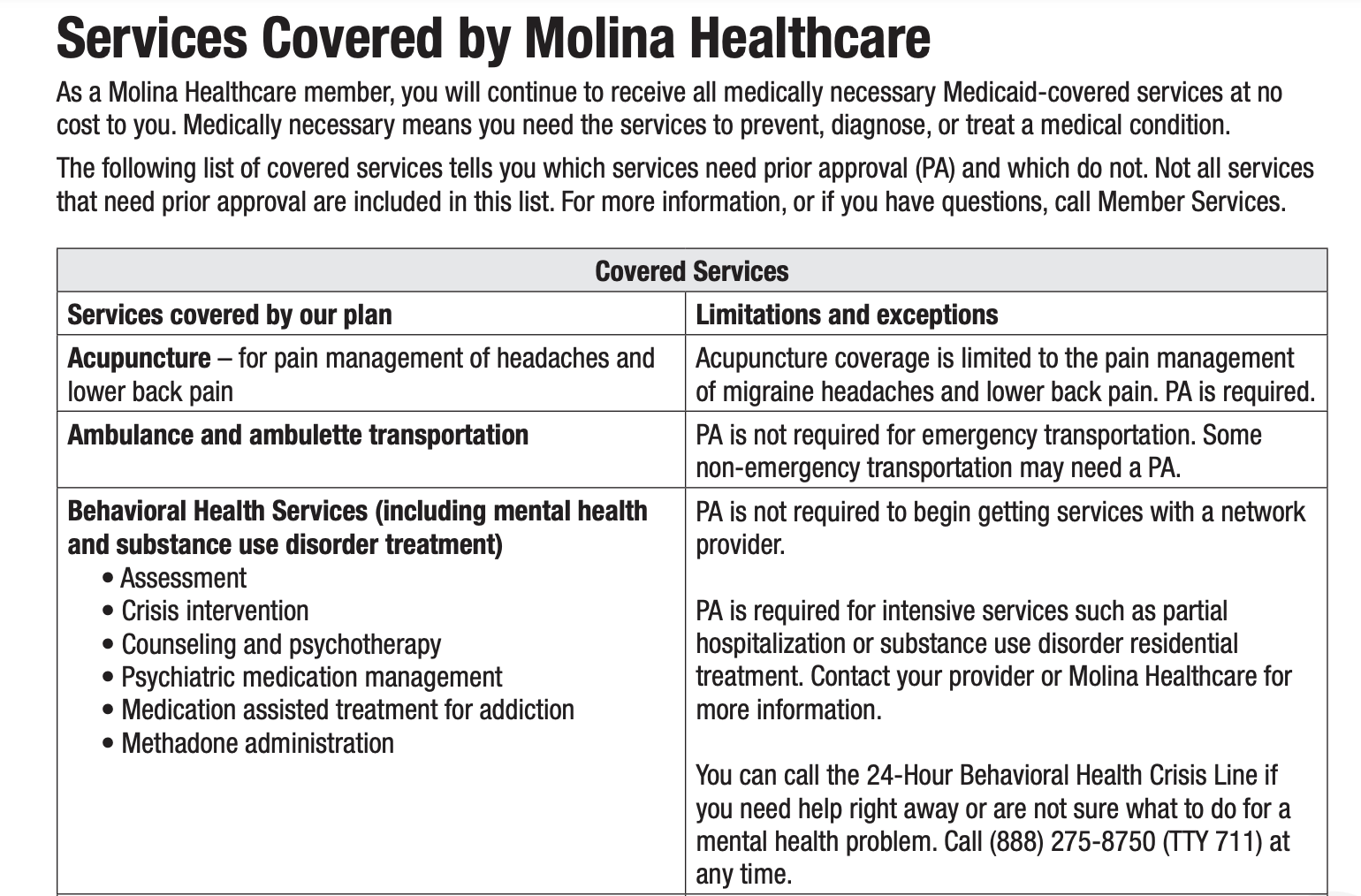
When you’re working with Molina Healthcare, it’s important to understand when a prior authorization is required and when it’s not. Not all behavioral health services trigger the need for a PA at Molina. Some services can be provided without first obtaining a PA.
Molina Healthcare does not require PAs:
To begin receiving services with an in-network behavioral health provider
Molina Healthcare DOES require PAs:
For all behavioral health “intensive services”
For all behavioral health partial hospitalization programs
For all residential addiction treatment programs
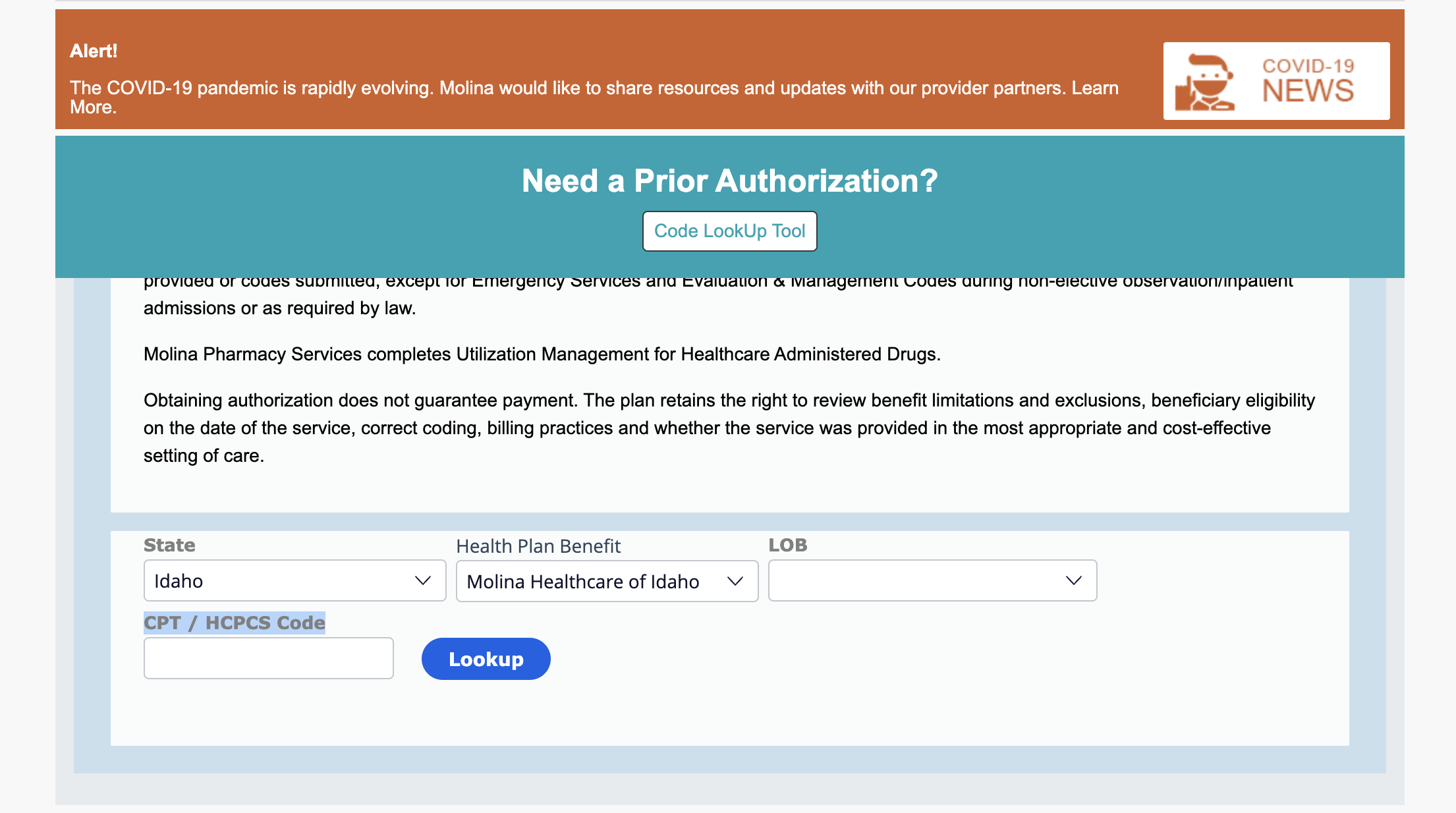
Not Sure if Your Addiction Treatment Center Needs a Prior Authorization? Try Using Molina’s Prior Authorization LookUp Tool
If you’re not sure if Molina will require a PA for your situation, you can always try using their handy online Prior Authorization LookUp Tool. Keep in mind that this tool is only for outpatient services, which means that you will not be able to verify the need for a PA for services that are considered inpatient services by Molina. In order to complete a search there, you’ll need:
The member’s state
The specific name of the member’s Molina plan
The LOB or line of business through which the member receives the plan (medicare, medicaid or marketplace)
The relevant CPT / HCPCS Code for the proposed treatment
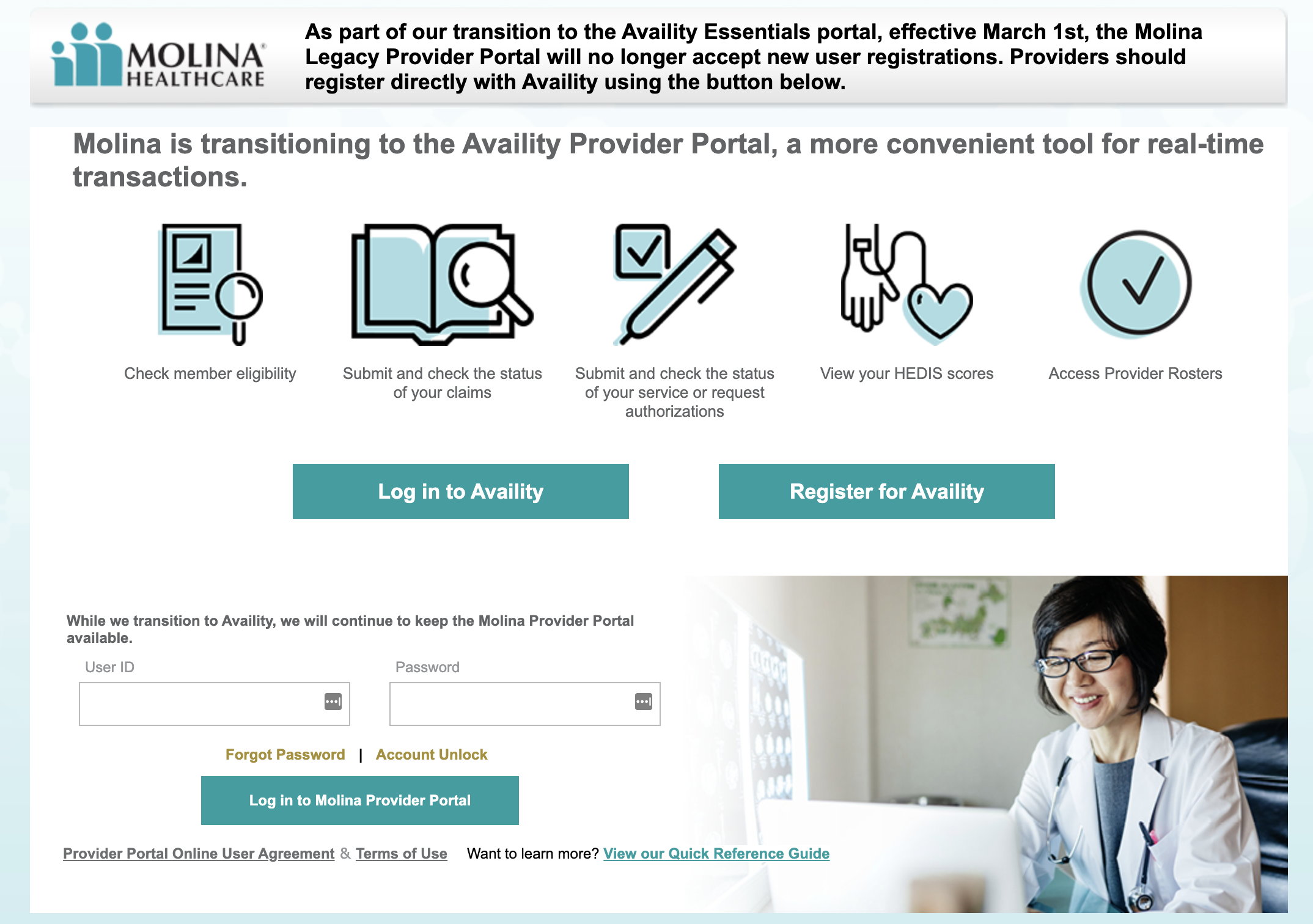
Need to Complete a PA with Molina Healthcare? Here’s the Login Page You Need to Get Started.
Molina is currently in the process of transitioning all of it’s billing business to a well-known third party healthcare billing software provider called Availity. If you need to complete a PA with Molina Healthcare - or do any billing work of any kind - you’ll need to register with Availity (If you haven’t already done so) and log into Availity’s Provider Portal.
Prefer a Paper Version of the Prior Authorization Form with Molina Healthcare for Addiction Treatment?
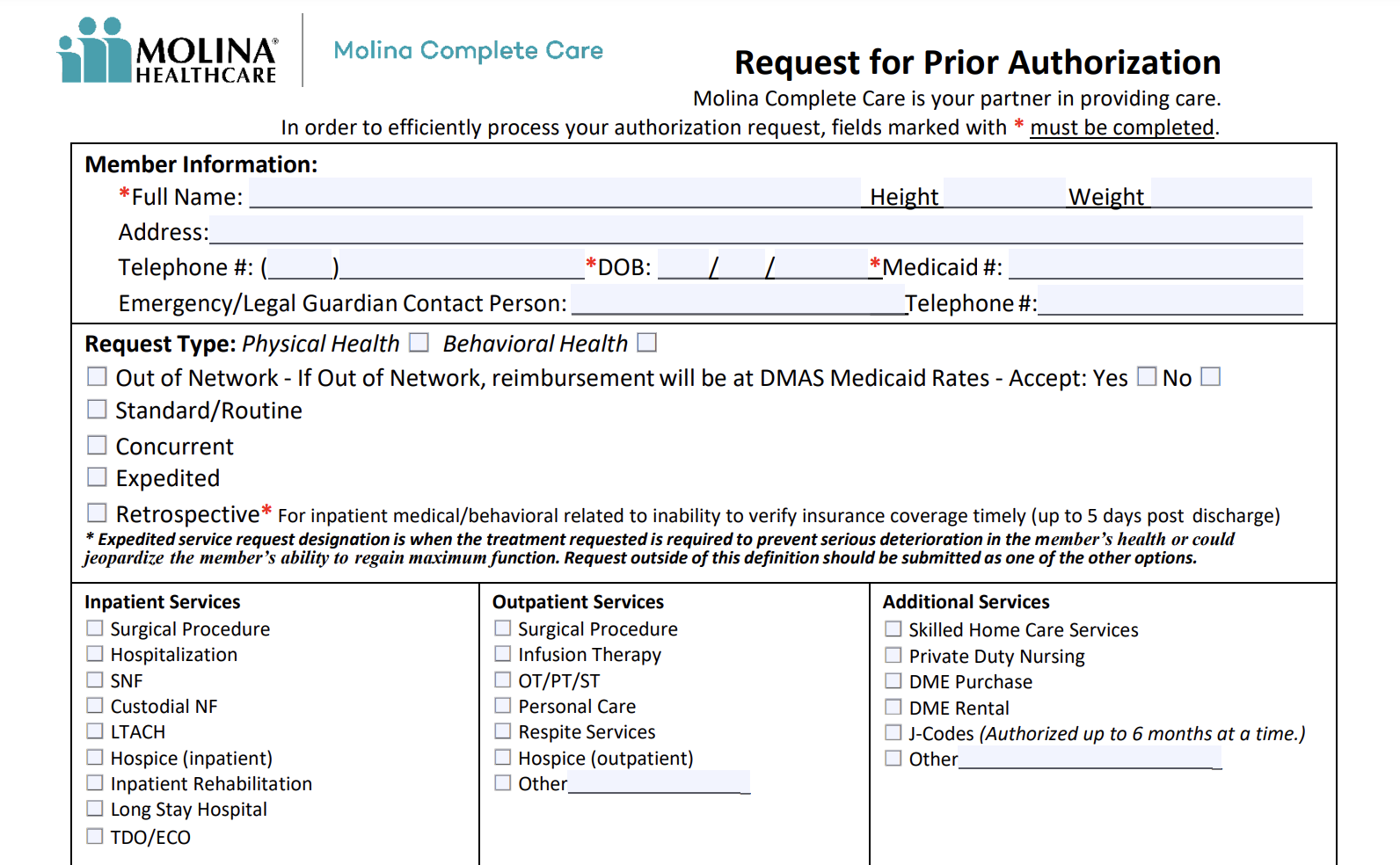
You’re in luck - here’s a link to Molina’s Request Prior Authorization Form. The easy-to-fill-out PDF can be quickly downloaded and processed the old fashioned way if you’d prefer to not tangle with Availity.
Fed Up With Prior Authorization Problems with Molina Healthcare? We Can Help.
Obtaining PAs with Molina Healthcare can be an expensive time waster for busy addiction treatment centers and providers.
BehaveHealth’s Revenue Cycle Management (RCM) service includes soup-to-nuts, hyper-detailed, hands-on attention to every single component of your addiction treatment billing needs. We have strong working relationships with every major insurance company in the United States.
Even better, we’re not health care generalists. We only work for behavioral health providers like you.
Let our team of specialists handle it all:
Verification of Benefits
Utilization Review
Billing and Collections
Patient Responsibility
Denials and Appeals
Get your free trial started today and see why more addiction treatment centers prefer Behave Health.