Premera - also known as Premera Blue Cross - is the largest health insurance payer in the Pacific Northwest. This Blue Cross Blue Shield Association affiliate is a nonprofit payer serving over 2 million members in Washington state and Alaska. They also happen to to be the recipient of the second largest HIPAA violation fine in United States history.
Like most health insurance plans, Premera is subject to parity laws which require them to cover behavioral health care and addiction treatment as equitably as they cover other health conditions. Still, patients have long complained of short inpatient stays for addiction treatment at Premera.
What Addiction Treatment Utilization Forms Are Required for Addiction Treatment Centers Working with Premera Blue Cross?
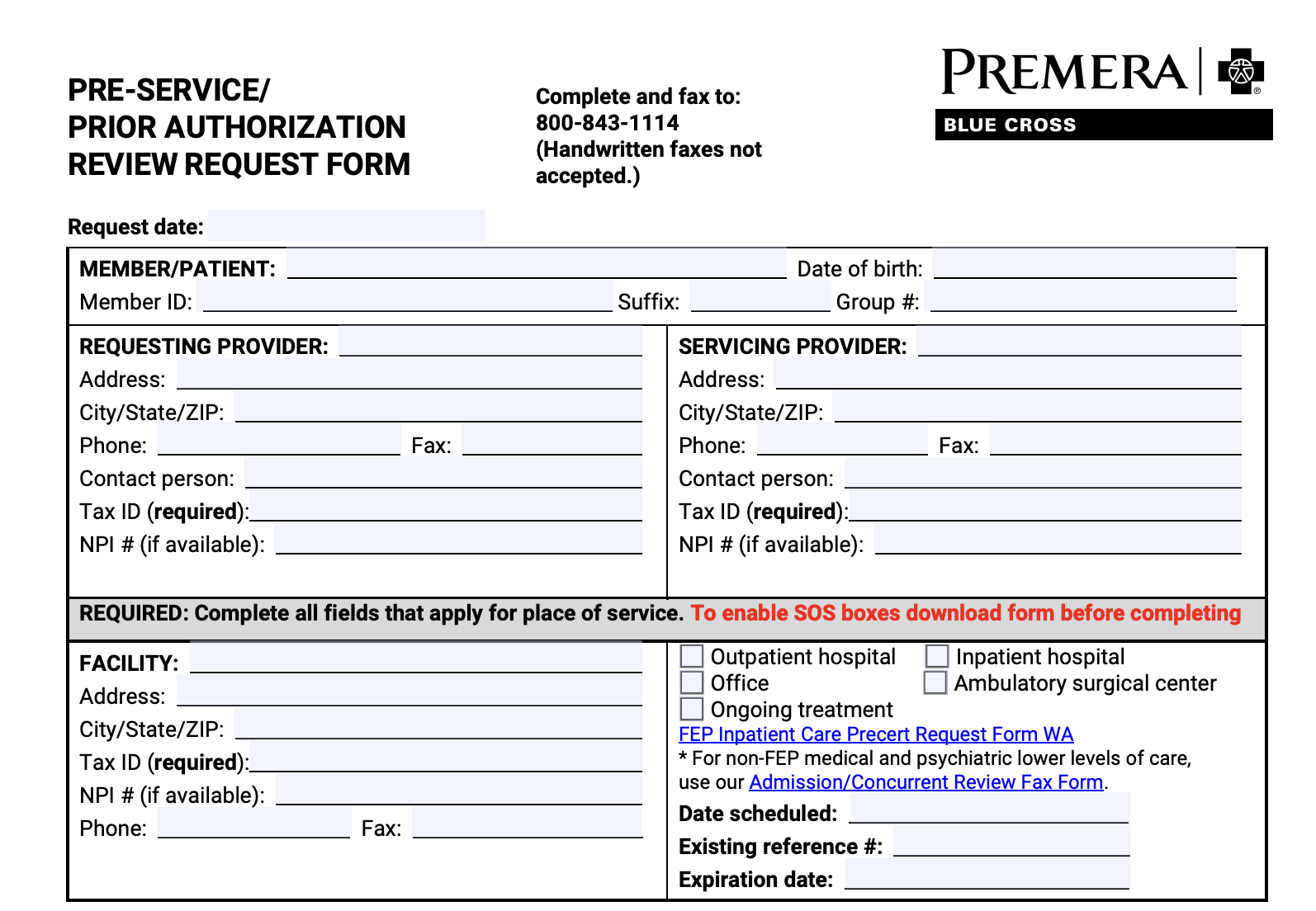
The primary form you’ll be required to fill out when dealing with Premera Blue Cross is the prior authorization request form.
There are several ways to complete this form.
Premera recently began asking providers to submit all prior authorization requests via Availity. You can register for Availity here. Premera says that submitting prior authorization request forms electronically through Availity ensures the fastest processing time possible. You can also check on prior authorization request status using Availity for the fastest real-time updates to processing.
Addiction treatment centers can also submit electronically completed prior authorization request forms to Premera via fax. In 2021, Premera Blue Cross stopped accepting all handwritten forms via fax, including any handwritten prior authorization request forms. This goes for in network prior authorization request forms and out of network requests, as well.
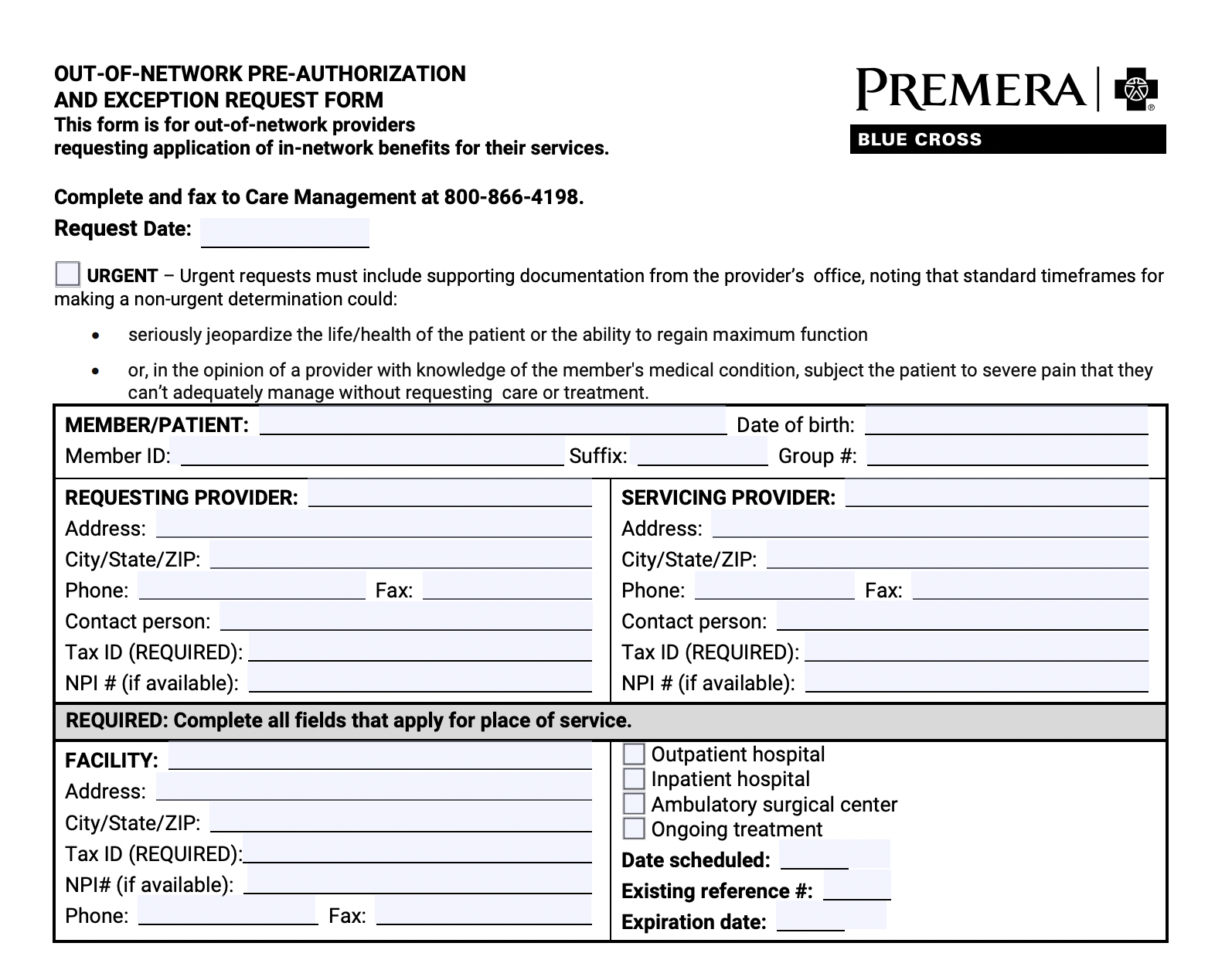
There Are Two Separate Prior Authorization Utilization Forms Addiction Treatment Providers Need for Premera Blue Cross
While most payers have only one prior authorization request form, Premera actually has two - one for in-network providers and another for out-of-network providers.
Premera’s Addiction Treatment Utilization Forms for In Network Providers
You can access the form for in network addiction treatment providers here.
Premera’s Addiction Treatment Utilization Forms for Out of Network Providers
You can access the form for out-of-network addiction treatment providers here.
You can also read more about all the rules that affect Premera’s prior authorization requests and utilization review processes on their website.
What Addiction Treatment CPT Codes Require Prior Authorization Utilization Forms With Individual Premera Blue Cross’ Plans?
You can find a list of all procedures and treatments requiring prior authorization at Premera Blue Cross here.
For individual plans, Premera requires prior authorization for the following types of addiction treatment:
Inpatient admission
Intensive outpatient hospitalization
Partial hospitalization programs
Residential treatment programs
You’ll know if a member has an individual plan if it says “individual plan” on the back of their membership card.
What’s missing from this list? Here’s the types of addiction treatment that do not require prior authorization for individual plans with Premera:
Outpatient addiction treatment
Emergency detox addiction treatment
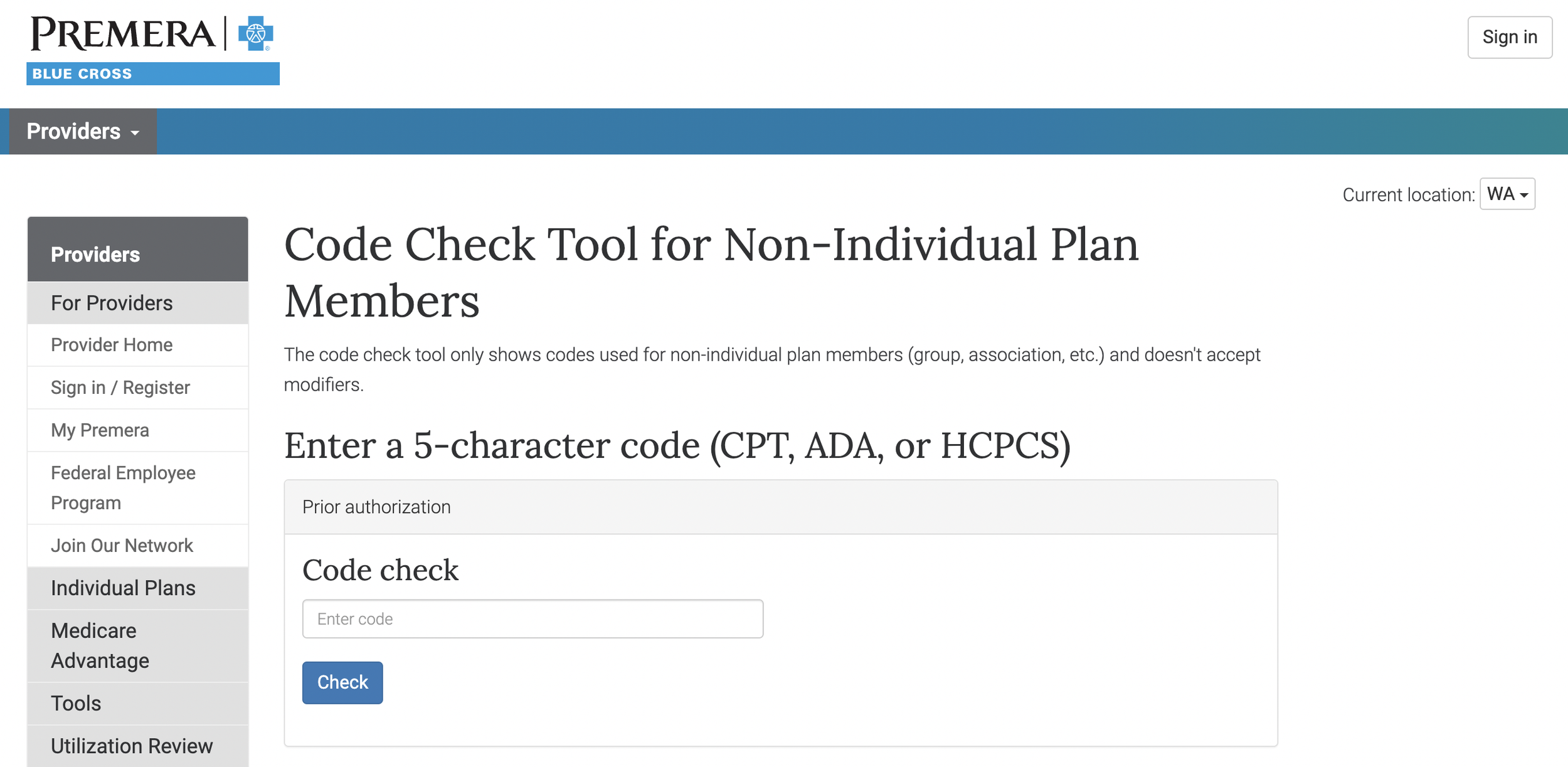
What Addiction Treatment CPT Codes Require Prior Authorization Utilization Forms With Non-Individual Premera Plans?
The term “non-individual plans” is somewhat confusing, but Premera simply uses this term to identify their medicare and medicaid plans.
For non-individual plans, you can use Premera’s code-check to tool to see if a given five character addiction treatment CPT code requires prior authorization with Premera or not.
According to Premera’s Clinical Review by Code List, the following addiction treatment CPT codes require “pre-service review,” which is another term for prior authorization:
H0008 - Subacute Detox, Hospital inpatient
H0009 - Acute Detox, Hospital inpatient
H0010 - Subacute detox, Residential program inpatient
H0011 - Acute Detox, Residential program inpatient
All decisions about coverage for these CPT codes are based in medical necessity.
Here’s a screenshot of the relevant portion of Premera Blue Cross’ Clinical Review by Code List:
Tired of Searching for Premera Blue Cross’ Addiction Treatment Utilization Forms? We Can Help.
BehaveHealth’s Revenue Cycle Management (RCM) service includes soup-to-nuts, hyper-detailed, hands-on attention to every single component of your addiction treatment billing needs. We have strong working relationships with every major insurance company in the United States.
Even better, we’re not health care generalists. We only work for behavioral health providers like you.
Let our team of specialists handle it all:
Verification of Benefits
Utilization Review
Billing and Collections
Patient Responsibility
Denials and Appeals
Get your free trial started today and see why more addiction treatment centers prefer Behave Health.