Today, we’ll look at what addiction treatment providers need to know about Highmark Inc, including what kind of addiction treatment services are covered by Highmark Inc, what the difference between pre-certification, prior authorization and authorization is at Highmark, what CPT codes require pre-certification at Highmark, as well as how to submit an addiction treatment precertification request at Highmark.
Who is Highmark Inc. and What Kind of Addiction Treatment Services Do They Cover?
Highmark Inc is a 18.2 billion dollar-a-year non-profit healthcare organization that provides services in West Virginia, Pennsylvania, Delaware and eastern Ohio. They operate as a complex conglomeration of various Blue Cross Blue Shield Association franchisees across multiple states, doing business as five different entities: Highmark Blue Cross Blue Shield (Western PA), Highmark Blue Shield (Central PA), Highmark Blue Cross Blue Shield West Virginia, Highmark Blue Cross Blue Shield Delaware and Highmark Health Options (Delaware).
In recent years, Highmark, Inc. has joined a growing number of health insurance payers interested in investment in virtual addiction treatment. Highmark Inc signed a deal with Ria Health to provide virtual alcohol use disorder treatment to members and they teamed up with axialHealthcare in Pennsylvania to treat general substance use disorder there virtually, as well.
Highmark Inc has focused most of its addiction treatment energy into prevention. They’ve worked on cutting back opioid prescription levels within their membership and making life-saving prescriptions like Naloxone more available to at-risk members. Despite operating in states with some of the more dire opioid overdose statistics, Highmark members experience 50% fewer opioid-related overdoses than the average American, probably owing to their restrictive opioid prescription policies.
What is the Difference Between Pre-Certification, Pre-Authorization and Authorization at Highmark, Inc?
While Highmark uses all three of these terms at different times, they all point to the same concept: requesting permission to grant billable treatment before providing services and admitting patients into care. These terms can be used interchangeably because they all mean the same thing at Highmark, Inc.
What Addiction Treatment Services Require Pre-Certification or Authorization at Highmark?
You can find a list of procedures requiring authorization (also known as pre-certification, prior authorization, prior auth or certification) in two places on Highmark’s website: at the general Provider Resource Center and on the Highmark Behavioral Health Provider Portal.
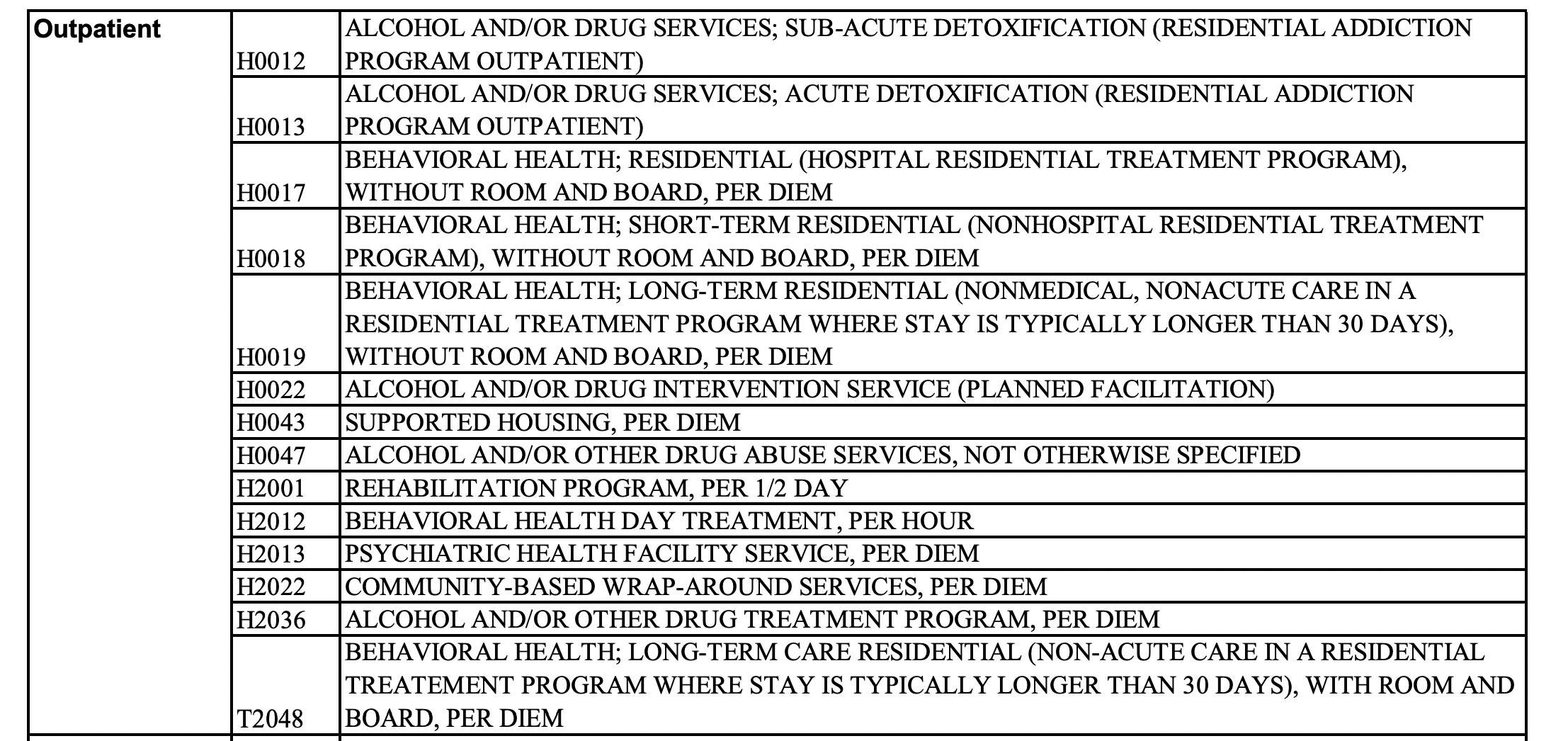
According to the PDF of procedures requiring authorization at Highmark, outpatient CPT addiction treatment codes that require authorization at Highmark include: H0012, H0013, H0017, H0018, H0019, H0022, H0043, H0047, H2001, H2012, H2013, H2022, H2036, and T2048. Inpatient, detoxification and rehabilitation CPT treatment codes that require authorization at Highmark include: H0008, H0009, H0010, H0011.
You can easily reference what CPT codes need authorization or precertification at Highmark using the screenshot of the relevant portion of the authorization list below, which is sorted into Outpatient addiction treatment CPT codes and Inpatient addiction treatment CPT codes:
How Do I Request Addiction Treatment Pre-Certification or Authorization with Highmark, Inc?
There are several ways to request pre-certification or authorization with Highmark.
Highmark encourages all providers to use the ACM functionality on the NaviNet system to submit authorization requests. You can access information about how to use the NaviNet system in Highmark’s Behavioral Health ACM Authorization Submission Manual.
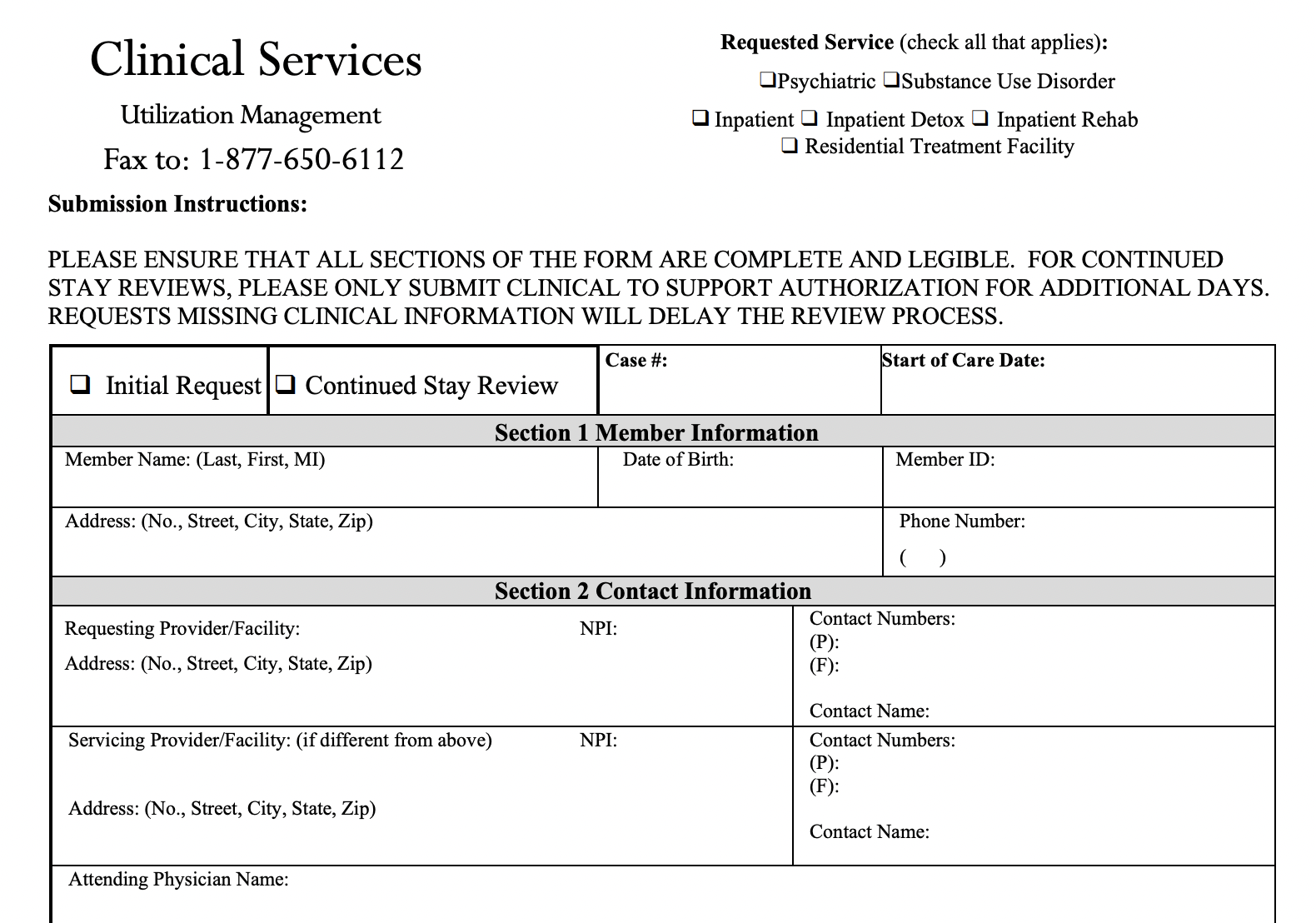
You can also fill out an old-fashioned authorization form and submit it to Highmark via fax.
Finally, if neither of these options are working for you, you can contact Highmark directly via phone to request authorization for addiction treatment services.
Each state and region has a different contact number for behavioral health pre-certifications.
Western Pennsylvania: 1-800-258-9808
Eastern, Northern and Southern Pennsylvania: 1-800-628-0816
Delaware: 1-800-421-4577
West Virginia: 1-800-344-5245
Still Confused About Pre-Certification and CPT Codes at Highmark, Inc? We Can Help.
BehaveHealth’s Revenue Cycle Management (RCM) service includes soup-to-nuts, hyper-detailed, hands-on attention to every single component of your addiction treatment billing needs. We have strong working relationships with every major insurance company in the United States.
Even better, we’re not health care generalists. We only work for behavioral health providers like you.
Let our team of specialists handle it all:
Verification of Benefits
Utilization Review
Billing and Collections
Patient Responsibility
Denials and Appeals
Get your free trial started today and see why more addiction treatment centers prefer Behave Health.