So you need to file an appeal on a claim decision from Anthem, Inc at your addiction treatment or behavioral health center but you’re not sure where to find the contact information necessary to do so?
Whether your coverage decision impacts patient admissions, continuing care or shift in level of care for the patient, it’s always frustrating to have to wrestle with insurance payers to give patients the care they need.
Today, we’ll talk about why so many providers like you find themselves seeking coverage decision appeals from Anthem and how to fast track those appeals to get expedited care for addiction treatment patients who need care ASAP.
Why Do So Many Addiction Treatment Providers Need to Wrestle with Anthem for a Favorable Coverage Decision?
We’ve written elsewhere about Anthem’s notoriously high denial rates for addiction treatment around the country. It’s no secret that Anthem has a track record of denying all types of health coverage - not just behavioral health coverage - at roughly twice the national average. That means if your patient has Anthem insurance, they are two times more likely to have coverage for their addiction treatment care denied. One study found that Anthem, Inc patients face an astonishing behavioral health claim denial rate of 90%. Even opioid use disorder patients found it difficult to seek coverage from Anthem, Inc, typically facing denial rates between 9.5% and 28.3%.
How Does Anthem Maintain Such a High Rate of Claims Denials With Addiction Treatment Patients?
Anthem Inc does the following things to keep successful behavioral health claims to a minimum:
Documentation requirements
Stringent prior authorization (PA) rules
Unusual hoops for physicians and other professionals to jump through
Denying physician-requested inpatient care in favor of less expensive levels of care
Frequent use of exclusions
Punishing patients for not securing prior authorization before receiving care
Etc, etc, etc (Anthem uses all of these tactics - and more - to deny coverage for behavioral health
When Can I File an Appeal with Anthem for a Bad Addiction Treatment Coverage Decision?
As a rule, all appeals need to be made within sixty days of the original decision. However, Anthem does allow for written requests to include information about why the appeal was not made within sixty days of the original denial if you find yourself appealing a decision that is over two months old. This scenario is rare in addiction treatment but it’s not completely impossible.
Here’s Where to Find Information on Expedited or “Fast” Appeals for Anthem’s Addiction Treatment Coverage Decisions
There is no “expedited appeal” line or special address to contact if you’re pursuing an expedited appeal at Anthem, Inc on behalf of a behavioral health patient. Your options for an expedited appeal are the same as for those of a standard appeal: you mail a written appeal to a physical address, call member services on the weekdays only or fax in your written appeal form. For most addiction treatment organizations, phoning in the expedited appeal will usually make the most sense. It’s important to get the patient into treatment as soon as they feel ready, as the window of opportunity is frequently very brief.
According to member services at Anthem, here’s where you want to send your expedited appeal:
Anthem Blue Cross Cal MediConnect PlanMMP Complaints, Appeals and Grievances4361 Irwin Simpson RoadMailstop OH0205-A537Mason, OH 45040
Or
1-855-817-5785 (TTY: 711)
Or
Fax number 1-888-458-1406
Here’s What to Include in Your Appeal with Anthem, Inc
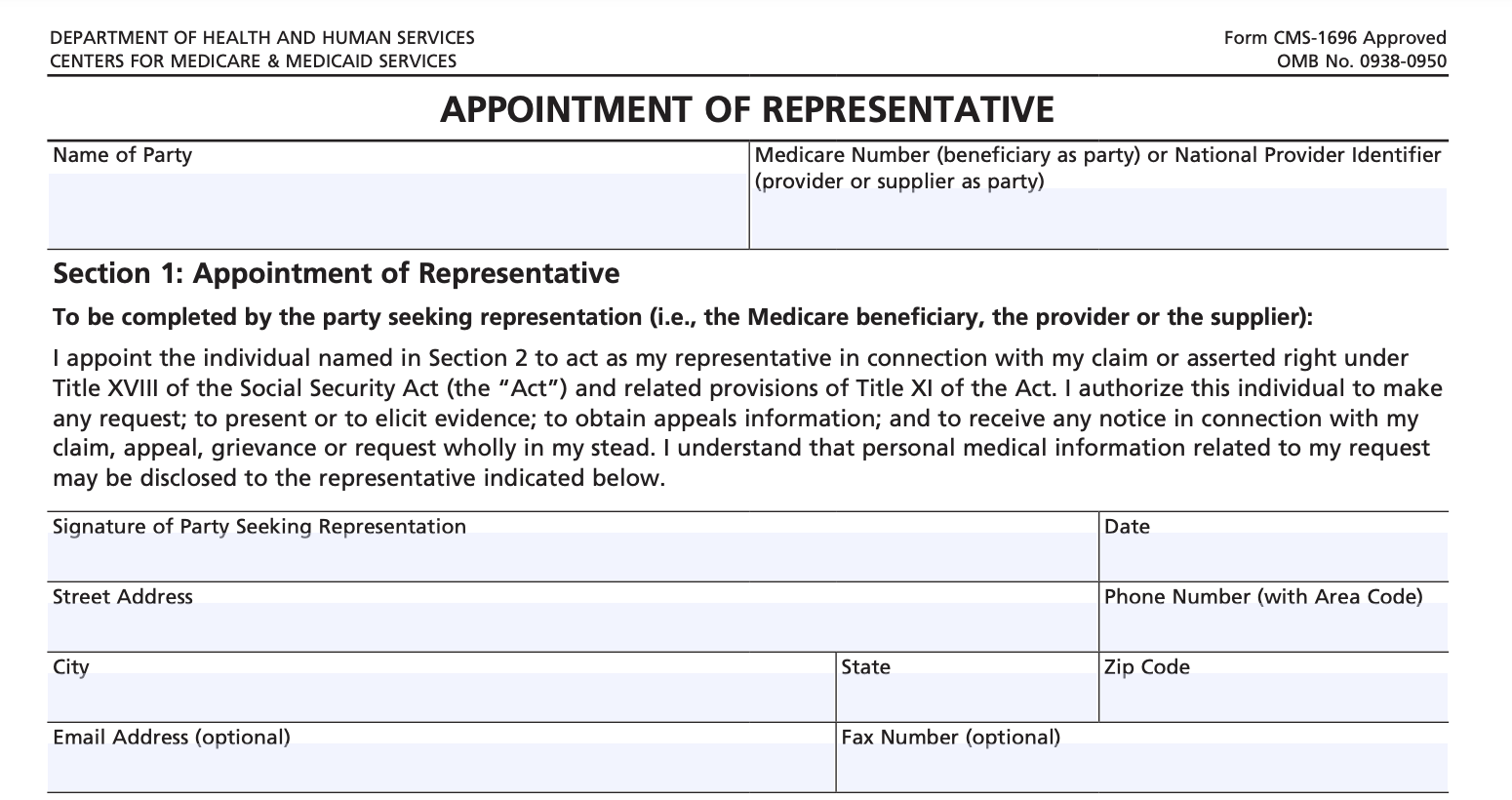
You’ll want to have the patient fill out the appointment of representative form that grants you permission to seek out an appeal on their behalf in the first place. You’ll also want to include:
The patient’s name, address and member ID number
The reason for the appeal
Additional evidence to back up your claim of medical necessity
The Appointment of Representative Form (if you’re appealing on behalf of another person).
Struggling With Expedited Appeals for Anthem Inc’s Addiction Treatment Coverage? We’re Here for You
Behave Health is committed to making it easier - and more profitable - to operate evidence-based, results-focused addiction treatment centers.
Get your free trial started today and see why more addiction treatment centers prefer Behave Health.
Need help with certification? Behave Health can also help direct you to the right resources for help with Licensing or Accreditation by either The Joint Commission or CARF. Mention to your product specialist that you’re interested in this service after you start your free trial!