We're excited to announce that Delaware's First State Alliance of Recovery Residences (FSARR) has teamed up with Behave Health for streamlined recovery residence certification across the state. This collaboration represents a major advancement in how Delaware recovery residence certification is managed, bringing digital efficiency to an essential process that ensures quality and safety standards throughout the recovery housing sector.
Modernizing FSARR Certification in Delaware
FSARR, Delaware's official NARR affiliate, now leverages the Behave Health Affiliate Management Platform (AMP) certification platform to digitize and simplify the entire certification workflow for recovery residences. With the implementation of House Bill 114, known as the Matthew D. Klosowki Act, certified recovery homes gain access to state referrals, public funding, and recognition as safe, compliant environments for individuals in recovery.
Our platform transforms how operators navigate Delaware sober living certification requirements by providing intuitive tools for application submission, document management, and compliance tracking—all within a secure, HIPAA-compliant digital environment.
What Behave AMP Brings to Delaware Recovery Residences
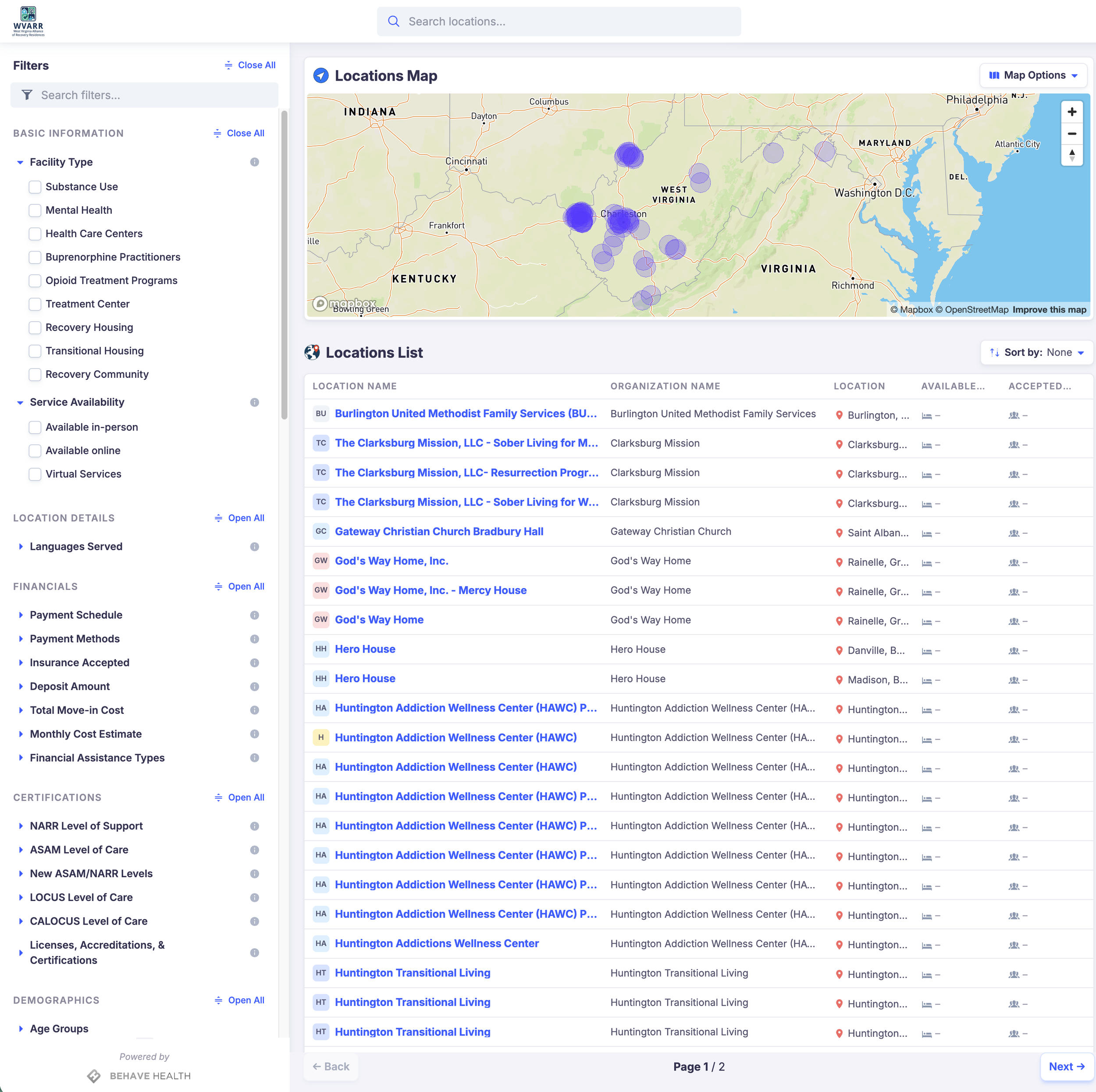
The Behave AMP platform offers comprehensive features specifically designed for FSARR recovery housing standards and certification needs:
Application Workflow Management: Efficiently submit and track certification applications from start to finish, reducing processing time significantly
Site Review Coordination: Streamlined scheduling and documentation for onsite inspections and compliance reviews
Grievances & Incident Management: Built-in systems for reporting and resolving complaints or safety events within the required 72-hour timeframe
Certified Organization Management: Real-time tracking of certification status, renewal dates, and compliance documentation
Communication Features: Direct messaging capabilities between FSARR and recovery residence operators for faster resolution of questions
How to Get FSARR Certified Using Behave AMP
Recovery residences seeking digital certification for recovery homes can now access FSARR's online portal powered by Behave Health. Operators submit documented policies, procedures, staffing credentials, and evidence of life skills programming directly through the platform, ensuring alignment with NARR's nationally recognized standards.
The platform guides applicants through requirements for safety protocols, resident rights, ethical operations, and level-appropriate oversight—whether operating as a monitored, supervised, or service provider residence.
Benefits for the Delaware Recovery Community
This Behave Health and FSARR collaboration delivers measurable advantages for all stakeholders:
Faster Certification: Reduced administrative burden accelerates approvals for compliant facilities
Enhanced Transparency: Real-time status updates keep operators informed throughout the process
Improved Compliance: Automated tracking ensures nothing falls through the cracks
Increased Confidence: Residents, families, and referral sources trust certified homes that meet rigorous standards
Scalability: As Delaware's recovery housing sector grows, Behave AMP supports FSARR's mission to certify all eligible residences statewide
About Behave Health's NARR Affiliate Management Platform
Behave Health developed the AMP platform in strategic alliance with the National Alliance for Recovery Residences (NARR) to provide state affiliates with specialized technology for certification management and data collection. Our solution reduces certification processing time while providing unprecedented real-time visibility into the recovery housing ecosystem.
The platform is already being adopted by multiple state affiliates, creating a unified digital infrastructure that elevates standards and outcomes across the national recovery residence network.
Join Delaware's Certified Recovery Housing Network
Recovery residence operators interested in FSARR certification can visit fsarr.org to begin their application process. FSARR not only certifies residences but provides guidance and support to help homes meet certification requirements.
For more information about how Behave Health's Affiliate Management Platform can support your state affiliate or recovery residence operations, visit behavehealth.com or contact our team at contact@behavehealth.com.
About Behave Health
Behave Health provides integrated EHR, CRM, ERP, and RCM solutions for behavioral health treatment centers, recovery residences, and affiliates nationwide. Our all-in-one platform streamlines operations, improves compliance, and enhances outcomes across the entire continuum of care.