Looking for an Addiction Treatment Billing Claims Address for Cigna?
If you’re a behavioral health provider, you probably don’t actually want a billing claims address for Cigna at all.
Addiction Treatment Centers Don’t Actually Need a Medical Billing Claims Address for Cigna
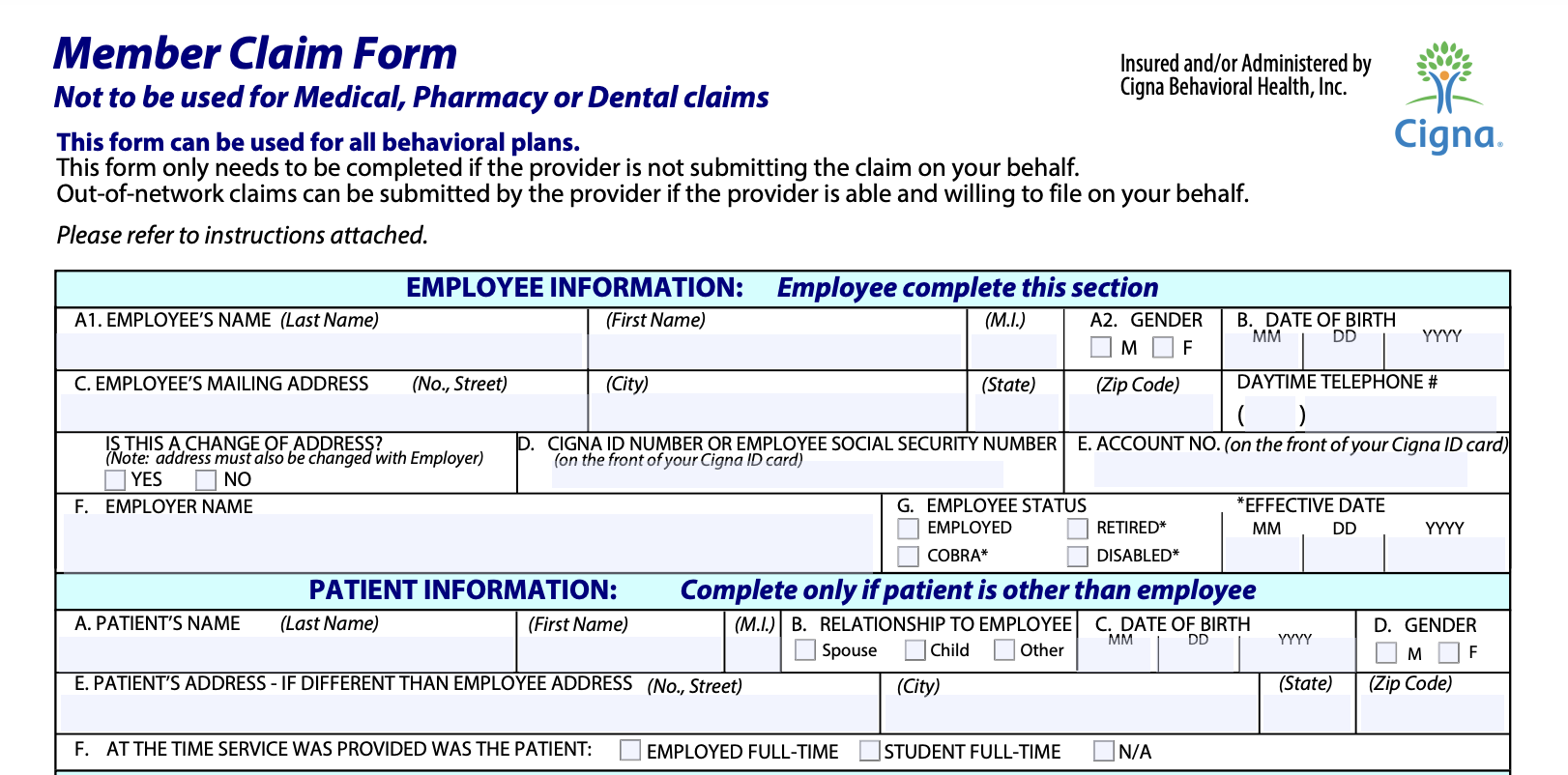
While individual Cigna members who are doing their own medical claims submissions do need a medical billing claims address to submit their Member Claim Form, addiction treatment centers and other behavioral health professionals don’t need to use paper claims at all.
In fact, Cigna doesn’t even accept old fashioned paper claims from medical professionals anymore.
If you’re looking for the billing claims address for Cigna as a private member submitting a behavioral health claim, you’ll want to use this address:
Cigna Behavioral Health, Inc.
Attn: Claims Service Dept.
P.O. Box 188022
Chattanooga, TN 37422
Note: Addiction treatment centers and behavioral health providers should NOT use this address. Read on to learn more about where to submit claims to Cigna as an addiction treatment professional.
Cigna Uses an EDI System for Electronic Billing Claims Instead of a Billing Claims Address for Addiction Treatment
Instead of paper billing and paper claims, Cigna encourages medical providers (like addiction treatment professionals) to use an Electronic Data Interchange, or EDI system, provided through one of several vendors that work with Cigna’s automated transfer data format. While many billing professionals associate EDIs with Medicare or government subsidized health plans, Cigna uses an EDI for all types of medical plans, including employer health plans and privately purchased health plans.
Cigna covers all of the ins and outs of using an EDI vendor on their How to Submit a Claim page, which goes over not only the claims submission process but also such topics as when to file a claim and what constitutes a “clean claim” for Cigna. You can also learn about how to submit electronic claims in Cigna’s proprietary (and free) Electronic Data Interchange (EDI) Electronic Claim Submissions eCourse.
How do I Get an EDI? Who are Some of the EDI Vendors Who Work with Addiction Treatment Billing Claims for Cigna?
Cigna will connect with any billing service that doesn’t charge the insurance giant for EDI transactions. Vendors must also be EHNAC HNAP-EHN accredited and CAQH Core Certified in order to be considered for direct connection. The following vendors are all compatible with Cigna electronic claims submissions:
Availity Gateway Services
Change Healthcare
Eligible Inc
Experian Health, Inc
Instamed
Nanthealth
Office Ally
PNT Data
SSI Group
TransUnion Healthcare, Inc
Trizetto Provider Solutions - Gateway EDI
Waystar Health
What are the Benefits of Electronic Claims Submissions for Addiction Treatment Billing with Cigna?
The primary benefits of using an EDI vendor to submit claims to Cigna is that the process saves time, paper and unnecessary paperwork expenses like stamps, printer cartridges, printing paper and other physical supplies and costs associated with traditional paper billing. EDIs also avoid the unnecessary faxing of forms, which is a huge boon to anyone working in a fax-saturated medical office.
Moreover, EDIs are able to screen for coding errors in a way that manual paper claims cannot. If anything about the claim needs to be edited, you can do so electronically without filling out an entirely new form and thus duplicating your efforts.
Finally, the largest benefit to addiction treatment billing departments is probably the ability to track claims as they travel through the review process. This allows you to monitor your claim status and adjust expectations as necessary.
Who is Cigna, Anyway? Why Do So Many Addiction Treatment Patients Have Cigna Health Insurance?
Cigna is one of the largest insurance companies in the United States. Actually, it’s one of the largest companies in the United States, period. In 2021, Cigna ranked number 13 on the Fortune 500 list by revenue. That makes sense, because in 2021, Cigna made a staggering 174.1 billion dollars in revenue.
Cigna comes in on top of a few other lists, as well, notably USA Today’s “Most Hated Companies” list. Cigna ranked in the top 10 of this notorious list in 2015 and again in 2018. While insurance companies are rarely well-loved in the United States, it appears that Cigna’s reputation with members and providers alike falls far below industry standard. One study found that over a third of Cigna members reported a “negative customer experience” in 2018. This widespread dissatisfaction is likely tied to a 2011 California Nurses Association finding that Cigna’s claim denial rates hover around an astonishing 39.6%.
Tired of Looking for Addiction Treatment Billing Claims Addresses and Fiddling with EDIs for Cigna? We Can Help.
You’re not the first addiction treatment professional to get fed up with billing.
BehaveHealth’s Revenue Cycle Management (RCM) service includes soup-to-nuts, hyper-detailed, hands-on attention to every single component of your addiction treatment billing needs. We have strong working relationships with every major insurance company in the United States.
Even better, we’re not health care generalists. We only work for behavioral health providers like you.
Let our team of specialists handle it all:
Verification of Benefits
Utilization Review
Billing and Collections
Patient Responsibility
Denials and Appeals
Get your free trial started today and see why more addiction treatment centers prefer Behave Health.