What is Health Care Service Corporation or HCSC?
HCSC is the 5th largest insurance company in the United States. It boasts over 16 million members.
HCSC is a licensee of Blue Cross Blue Shield (BCBS) in five states: Illinois, Montana, New Mexico, Oklahoma, and Texas. HCSC is a specific type of nonprofit organization, and calls itself both a “customer-owned company” and a “mutual legal reserve company.” However, the company’s non-profit status has been called into question with lawsuits alleging that the company hoards cash and pays unusually large bonuses to executives rather than using surplus funds for the common good of policyholders.
HCSC also has a spotty record in providing its members adequate access to behavioral healthcare. In 2019, HCSC was named in a federal lawsuit which alleged that the company inappropriately denied behavioral healthcare claims in defiance of American Psychiatric Association guidelines.
What are Utilization Reviews or URs?
UR is a popular medical abbreviation for “utilization review,” sometimes also called utilization management.
Utilization reviews are performed by insurance companies to verify that addiction treatment is medically necessary and that it’s being performed at the appropriate level of care. Utilization reviews are considered to be an important component of managed care or value based care because it is one of the tools that insurance companies use to reduce costs while ensuring that evidence-based criteria are met in patient care.
In addiction treatment billing, utilization reviews most commonly come up when a patient is beginning, continuing, or extending care in an inpatient setting, but this is not always the case. There are many situations where utilization reviews are necessary in addiction medicine.
There are three different types of utilization reviews: prospective, concurrent and retrospective. Each of these refer to the timing of the UR.
Prospective URs take place before services are rendered. These are sometimes also referred to as the prior authorization process or PA.
Concurrent URs take place as care is being provided. Concurrent URs are not ideal because they can leave providers vulnerable to claims denials and patients liable for higher patient responsibility payments. Most addiction treatment centers avoid concurrent URs where possible.
Retrospective URs take place after care has already been completed. Like concurrent URs, retrospective URs are not ideal from a medical billing and revenue cycle management point of view, for largely the same reasons.
What Diagnosis Codes Should I Use for Addiction Treatment URs?
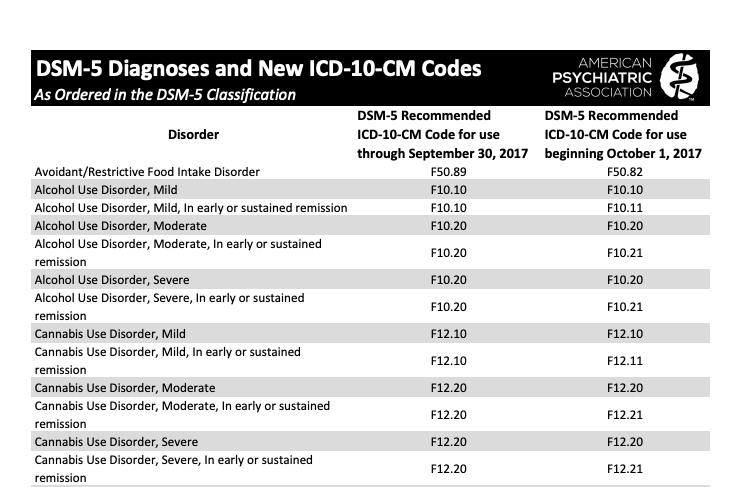
You can find a complete list of addiction treatment diagnosis codes (also know as ICD-10-CM codes) at the American Psychiatric Association. Each disorder is separated by drug of choice (i.e. alcohol, cannabis, opioids, amphetamines, cocaine, etc) and also coded by the intensity of the disorder.
For example, Opioid Use Disorder can be classified in the DSM V in six different ways: Mild, Mild and in early or sustained remission, Moderate, Moderate and in early sustained remission, Severe, and Severe and in early or sustained remission. Clearly, patients who need inpatient care will mostly fall into the Moderate or Severe category.
While they are classified differently, the diagnosis code for Moderate and Severe Opioid Use Disorder is the same: F11.20.
What Diagnosis Codes for Addiction Treatment Should I Avoid When Preparing URs for Health Care Service Corporation?
Because HCSC has a history of denying addiction treatment claims by using overly restrictive guidelines that contradict the APA’s clinical opinion, it is critical that you code your UR appropriately. Be sure that you use the diagnosis code that most effectively reflects the patient’s condition. If the patient’s condition is acute, but sure that the diagnosis code reflects that. Avoid accidentally using diagnosis codes that indicate that the patient’s condition is mild or in early or sustained remission.
For example, the following codes are likely to not “pass” inpatient addiction treatment URs with Health Care Services Corporation:
F10.10
F11.10
F13.10
F15.10
F14.10
F15.10
Confused by the UR Process for Addiction Treatment with HCSC? We Can Help.
You’re not the first addiction treatment professional to get fed up with billing.
BehaveHealth’s Revenue Cycle Management (RCM) service includes soup-to-nuts, hyper-detailed, hands-on attention to every single component of your addiction treatment billing needs. We have strong working relationships with every major insurance company in the United States.
Even better, we’re not health care generalists. We only work for behavioral health providers like you.
Let our team of specialists handle it all:
Verification of Benefits
Utilization Review
Billing and Collections
Patient Responsibility
Denials and Appeals
Get your free trial started today and see why more addiction treatment centers prefer Behave Health.