Who Is Aetna and What Do They Have to Do With Addiction Treatment?
Aetna is a major insurance payer in the addiction treatment field. A subsidiary of CVS Health, Aetna is a managed health care company - in other words, a health insurance company - that boasts over 22.1 million members per year.
Aetna has stringent standards for behavioral health coverage that some recent class action lawsuits allege stand in violation of the Health Parity and Addiction Equity Act, which states that behavioral health coverage must be treated as all other health condition coverage rules are. Also of note to addiction treatment providers, Aetna is also being sued for underpaying out-of-network claims, leading to large - and often uncollectable - patient responsibility payments.
In recent years, Aetna has put a large focus on virtual behavioral health care. For example, the company claims that they covered over ten million virtual behavioral healthcare sessions in 2021.
What is Precertification and When Does Aetna Require it for Addiction Treatment Centers?
Aetna uses the terms precertification and preauthorization interchangeably. Their insurance term glossary also refers to this concept as:
Authorization
Certification
Prior authorization
Pre-service utilization review (in Texas only)
Each of these terms means the same thing to Aetna, as it does to many players in the health insurance world.
Precertification is the process whereby a member or a healthcare provider acting on behalf of a patient asks for permission from the insurance company before seeking or administering treatment. This process also involves checking that the specific treatment is covered for the patient, and, if so, what that coverage entails.
Aetna generally requires addiction treatment centers - both “participating providers” and out-of-network providers - to obtain precertification before admitting patients.
What Addiction Treatment CPT Codes Require Precertification with Aetna?
According to Aetna’s Behavioral Health Precertification List, the following services, assuming they are even covered by the individual’s plan, always require precertification or authorization:
Applied behavioral analysis
Inpatient admissions
Partial hospitalization programs (PHPs)
Residential treatment centers admissions (RTC)
Transcranial magnetic stimulation (TMS)
In terms of how these services might translate into CPT codes, it’s overly simplistic to generalize about what specific set of codes may be used in what level of care, as certain components - such as case management, group counseling and laboratory analysis - will vary from program to program.
However, some generalizations can still be made.
For example, inpatient admissions for addiction treatment are usually represented by the codes:
Residential Treatment Center Admissions (RTC) might be represented by the following CPT codes, depending on the situation:
Finally, Partial Hospitalization Programs might be most often represented by the following addiction treatment CPT codes:
What Addiction Treatment CPT Codes Don’t Require Precertification with Aetna?
Some state and/or federal laws prohibit Aetna from requiring preauthorization for certain addiction treatment services.
According to their Behavioral Health Precertification List, beginning in 2019, Aetna had to discontinue their preauthorization requirements for:
Intensive outpatient
Outpatient detoxification (aka ambulatory withdrawal management)
Translated into addiction treatment CPT codes, there should be no in-network precertification requirement from Aetna regarding:
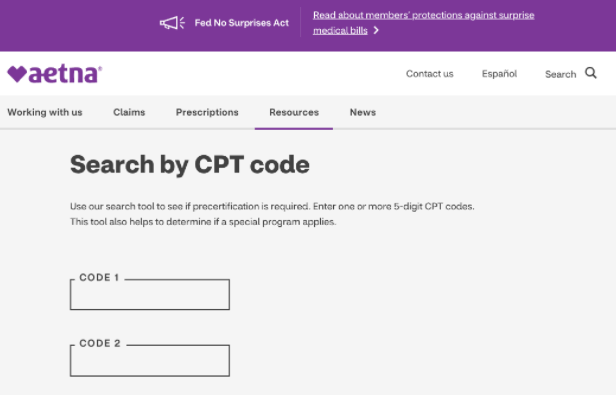
What About the “Search by CPT Code” Function on Aetna’s Precertification Information Page? Is That Reliable for Addiction Treatment Providers?
Aetna has a handy “search by CPT code” function on its website that claims it will scan a CPT code and let you know if that code requires a precertification or not. Unfortunately, while this would be very convenient, it is not reliable for addiction treatment providers.
When entered into Aetna’s search tool, all addiction treatment CPT codes come back with a “precertification not required” statement, which is very misleading.
If you continue to read the message, you’ll see that at the bottom, Aetna includes a message that says (emphasis added):
The procedure code you entered was not found on the Aetna Participating Provider Medical Precertification List. If you’re a participating provider, no precertification is required when this service is performed as an outpatient procedure for a medical or surgical diagnosis. This procedure code may require precertification for behavioral health diagnoses.
In other words, the search by CPT code feature is meaningless for behavioral health diagnoses, even when the CPT codes being searched are only used in the real world in connection with specific behavioral health diagnoses.
Our recommendation? Don’t rely on the “search by CPT code” function to determine if you need to seek a precertification for addiction treatment with Aetna.
Confused About Aetna’s Precertification Requirements for Addiction Treatment? We Can Help.
You’re not the first addiction treatment professional to have questions about addiction treatment billing.
The process changes constantly and requires an extraordinary attention to detail.
BehaveHealth’s Revenue Cycle Management (RCM) service includes soup-to-nuts, hyper-detailed, hands-on attention to every single component of your addiction treatment billing needs. We have strong working relationships with every major insurance company in the United States.
Even better, we’re not health care generalists. We only work for behavioral health providers like you.
Let our team of specialists handle it all:
Verification of Benefits (this process includes a PA)
Utilization Review
Billing and Collections
Patient Responsibility
Denials and Appeals
Get your free trial started today and see why more addiction treatment centers prefer Behave Health.