PHP stands for Partial Hospitalization Program. This type of care is used most in the behavioral health industry for treatment of substance abuse issues. It is also utilized for patients with mental health disorders. This guide explains the partial hospitalization program (PHP) level of care for behavioral health and addiction treatment providers, including clinical criteria, state requirements, and billing fundamentals.
Most state licensing departments classify PHP as an outpatient service, requiring an outpatient license, though, some states may classify PHP as inpatient. PHP can be either 5 days or 7 days per week and normally consists of at least 5 hours per day of programming.
PHP is often used after a Residential care program to acclimate the client to life outside of residential treatment. Depending on the program, they can be encouraged to look for employment in this level of care, but that is not a requirement. In early recovery, it is important to maintain structure for the client, which can be achieved with PHP. PHP keeps them busy for 5-6 hours per day, but also allows time for other things such as; employment, attending 12 step meetings, etc. PHP is less restrictive than residential care, but provides for less idle time than Intensive Outpatient, which is typically only three hours per day.
Get your free trial started today and see why more addiction treatment centers prefer Behave Health.
Partial Hospitalization Program (PHP) Level of Care: Requirements, Billing, and Benefits
Partial Hospitalization Programs (PHPs) provide a high-intensity, structured outpatient level of care for individuals who need more support than traditional therapy but do not require 24/7 inpatient hospitalization. PHPs are commonly used in mental health and addiction treatment to bridge the gap between inpatient care and routine outpatient services. In a PHP, patients attend treatment for several hours a day (often five days a week) and return home in the evenings, allowing them to receive intensive therapy while maintaining some daily routines. This article explores what PHPs entail, PHP requirements in key states like Texas, Florida, and California, how partial hospitalization billing and insurance reimbursement work (including important CPT/HCPCS codes), the patient experience and benefits of PHP, and ways to optimize your PHP program’s operations. We’ll also highlight internal resources (like guides on starting a PHP program and billing codes) and include external references from authoritative sources.
What is a Partial Hospitalization Program (PHP)?
A Partial Hospitalization Program (PHP) is a form of intensive outpatient treatment designed for patients who need structured care almost equivalent to inpatient treatment, but on a daytime-only basis. PHP stands for Partial Hospitalization Program. Key characteristics include:
Intensive Schedule: PHPs typically run 5 days per week (and sometimes 7), with at least 5 hours of treatment per day. Patients participate in a full day of therapy, counseling, and skills-building activities, then leave to spend evenings and nights at home or in community housing.
Outpatient Classification: In most states, PHP is licensed as an outpatient service (even though the care intensity is high). Patients are not admitted to a hospital; instead, they attend a clinic or treatment center daily. (Notably, a few states may classify PHP as inpatient, but this is the exception rather than the rule.)
Multidisciplinary Care: Treatment in a PHP involves a team of professionals. Typically, a psychiatrist serves as the medical director overseeing the program, and each patient has an attending psychiatrist responsible for their care. Licensed therapists provide group and individual therapy (and often family therapy), and nursing staff are present to monitor vitals, administer medications, and manage any side effects or medical issues. This comprehensive team approach ensures medical and psychosocial needs are addressed collaboratively.
Structured Treatment Plans: PHPs deliver structured, evidence-based interventions throughout the day. A patient’s week in PHP might include individual psychotherapy sessions, multiple group therapy sessions (covering topics like coping skills, cognitive-behavioral techniques, relapse prevention, etc.), psychiatric medication management, psychoeducation classes, and recreational or occupational therapy. Programs often incorporate behavioral health therapies, addiction counseling, and skill-building workshops to support recovery.
Target Populations: PHPs treat individuals with serious mental health conditions (such as major depression, bipolar disorder, anxiety disorders, or PTSD) and/or substance use disorders who need daily monitoring and support but are stable enough to live outside a hospital. It is also common for PHP mental health programs to support patients with co-occurring disorders (dual diagnosis). PHP can serve as a step-down from inpatient hospitalization – helping patients transition back to community life after a psychiatric hospital stay or residential rehab – or as a preventive step-up from standard outpatient care to avoid a full hospitalization.
Duration of Care: While length of stay varies by individual, many PHPs are short-term programs (e.g. 2-6 weeks of intensive treatment). The goal is to stabilize the patient, improve coping skills and symptom management, and then step down to a less intensive level of care (such as an Intensive Outpatient Program or weekly therapy). However, there is flexibility based on progress; some patients may participate in PHP longer if clinically needed, while others might transition out sooner.
In summary, PHP offers hospital-level therapy on an outpatient basis, providing an intermediate level of care that is more intense than regular outpatient therapy but less restrictive than inpatient hospitalization. This level of care is crucial for supporting individuals in acute phases of mental health or addiction recovery, ensuring they get structured daily treatment without completely disrupting their home life.
State-Specific PHP Requirements (Texas, Florida, California)
Regulations and licensing requirements for PHPs can vary by state. While most states regard PHP as an outpatient service, there are important state-specific rules about licensing, staffing, and operations. Below we overview PHP considerations in Texas, Florida, and California – three states with significant behavioral health industries and regulatory frameworks for PHPs.
PHP in Texas: Licensing and Guidelines
In Texas, a Partial Hospitalization Program is generally considered an outpatient program, but providers must navigate state-specific licensing rules, especially for substance use treatment services. Texas law requires chemical dependency treatment programs (which would include PHPs treating substance use disorders) to be licensed by the state unless an exemption applies. According to the Texas Health and Safety Code (Chapter 464): “A person may not offer or purport to offer chemical dependency treatment without a license… unless the person is exempted under Subchapter C.”. In practical terms, this means if you plan to operate a PHP in Texas for addiction treatment, you must obtain a license from the Texas Department of State Health Services. (One notable exemption in Texas is if you are an individual practitioner providing counseling without advertising as a treatment program, you might not need a facility license – but the moment you establish a program offering PHP-level care, licensure is required.)
For mental health PHP programs (not specifically treating substance abuse), you’ll still likely need to be licensed as an outpatient mental health facility or clinic, especially if providing intensive services. Texas typically classifies PHP under outpatient mental health services, so organizations should ensure compliance with any Texas Health and Human Services Commission regulations for psychiatric outpatient programs. Additionally, state guidelines emphasize proper medical oversight. The Texas Society of Psychiatric Physicians’ guidelines for PHP recommend having a psychiatrist medical director and require that each patient is under the care of an attending psychiatrist. There should be appropriate staff (therapists, nurses, etc.) to provide therapy, monitor vitals and medications, and handle emergencies on-site. Ensuring these clinical standards not only meets regulatory expectations but also aligns with best practices for patient care.
Internal Resource: If you are looking to start a PHP or IOP program in Texas, be sure to conduct a feasibility study and understand the competition. Behave Health offers a detailed guide on turning a group practice into an outpatient IOP/PHP facility in Texas, which covers business planning, zoning, staffing, and the Texas licensing process. This resource can walk you through the step-by-step requirements, including getting your program licensed in Texas and accredited.
PHP in Florida: Licensing and State Standards
Florida is known for its large number of addiction treatment and mental health facilities, and Partial Hospitalization Programs are a common level of care offered. In Florida, PHPs are generally considered day-treatment programs (a form of intensive outpatient service). State law in Florida mandates that any provider offering substance abuse treatment services (including PHPs for addiction) be licensed under Florida’s Department of Children and Families (DCF). The Florida Statutes (Title XXIX, Chapter 397) explicitly state that it is unlawful to act as a substance abuse service provider without a license under that chapter. In other words, if your PHP involves treatment of substance use disorders or co-occurring disorders, you must obtain the appropriate license from DCF’s Substance Abuse Program Office. This typically involves meeting specific staffing qualifications, safety standards, and program guidelines defined by Florida administrative rules.
Florida distinguishes some levels of care in its licensing categories. A PHP might fall under what Florida calls “Day or Night Treatment with Community Housing” if the program provides housing (sober living environment) alongside day treatment, or simply “Day Treatment” if no housing is provided. Ensure you apply for the correct service component license. The program will need policies in place for medical oversight, as Florida likely requires a physician or psychiatrist involvement for higher levels of care, and proper client-to-staff ratios for therapy services.
Additionally, Florida’s behavioral healthcare landscape is highly competitive. The state’s pro-business environment and reputation as a recovery destination have led to thousands of outpatient treatment programs. To stand out, a PHP in Florida must not only be fully compliant with DCF regulations but also demonstrate quality and unique value (specialized programs for certain populations, evidence-based practices, etc.). Keep in mind that payors in Florida often have utilization review processes for PHP – for example, securing prior authorization from insurance (including Florida Medicaid or private insurers like Florida Blue) is usually necessary before admitting a patient to PHP level of care. It’s wise to develop a strong utilization review and billing process (or use software like Behave’s RCM tools) to manage authorizations and documentation for medical necessity.
Internal Resource: For more information on operating in Florida, see our comprehensive guides such as insurance billing in Florida for addiction treatment and opening an addiction treatment center in Florida. These guides (available on the Behave Health blog) detail Florida’s regulatory environment, including working with insurers like Florida Blue and navigating Chapter 397 licensing.
PHP in California: Licensing and Certification Requirements
In California, the regulatory environment for PHPs has evolved in recent years to increase oversight of outpatient treatment programs. California now requires licenses for any facility providing addiction treatment services like PHP or IOP. Specifically, the California Department of Health Care Services (DHCS) mandates that any provider offering “detoxification, individual or group counseling, educational sessions, or alcoholism/drug abuse recovery or treatment planning” must be licensed – which encompasses PHP services. If you plan to run a PHP in California (for mental health or substance use), you will need to complete an application with DHCS to become a certified outpatient program. This involves submitting the Initial Treatment Provider Application to DHCS and paying the requisite fees (How to Turn Your Group Practice into an Addiction Treatment Outpatient Facility Offering IOP/PHP in California — Behavehealth.com).
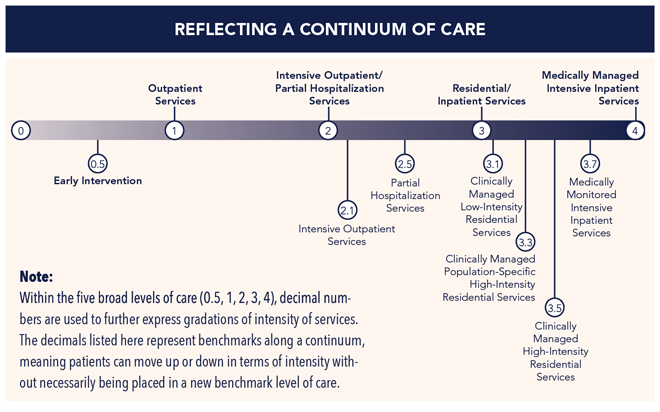
Moreover, California has an additional requirement: obtaining a Level of Care designation. California Health & Safety Code §11834.015 requires programs to have at least one DHCS-issued level of care designation and/or an ASAM (American Society of Addiction Medicine) level of care certification. For a PHP offering behavioral health or addiction treatment, this typically means aligning with ASAM Level 2.5 (Partial Hospitalization) criteria. ASAM Level 2.5 corresponds to roughly 20 or more hours of service per week and signifies a high-intensity outpatient service. Programs might seek ASAM Level of Care certification or accreditation (e.g., via CARF or The Joint Commission) to demonstrate they meet national standards for PHP level care.
Staffing in California PHPs must include appropriately licensed clinicians. If you’re a group practice transforming into a PHP, California may require that you have an LPHA (Licensed Practitioner of the Healing Arts) on staff (such as a licensed psychologist, LCSW, LMFT, or licensed counselor) who can sign off on treatment plans. Additionally, ensure compliance with any California laws regarding patient ratios, documentation, and reporting outcomes to DHCS. California’s focus on patient safety and quality means PHPs should maintain thorough performance improvement and utilization review processes, similar to inpatient programs, overseen by medical leadership.
Internal Resource: For a deep dive into California’s requirements, refer to our guide “How to turn your group practice into an outpatient IOP/PHP facility in California.” It walks through the licensing steps with DHCS, the need for an LPHA and other key personnel, and considerations like location and zoning in California. Additionally, if you’re starting a new program, you might find our checklist on opening a rehab center in California useful (covering everything from state applications to obtaining accreditation and payer contracts).
Partial Hospitalization Billing, CPT Codes, and Insurance Reimbursement
Understanding partial hospitalization billing is crucial for a PHP program’s financial health. Unlike regular outpatient therapy (billed per session code), PHPs usually bill on a per-day (per diem) basis using specialized codes that encapsulate the day’s worth of services. Proper coding and documentation ensure you get reimbursed by insurers for this intensive level of care. Below we outline common PHP billing codes and key points about insurance reimbursement for partial hospitalization.
Common PHP Billing Codes (HCPCS/CPT)
Partial Hospitalization Programs often use HCPCS Level II codes (sometimes referred to as CPT codes colloquially) that denote a day of intensive services. The exact code can depend on the payer and whether the focus is mental health or substance abuse treatment. Important codes include:
H0035 – Mental health partial hospitalization, treatment, less than 24 hours. This HCPCS code is widely used to bill for mental health PHP services on a per diem (daily) basis. It covers a structured day of psychiatric care, including therapy and other services. H0035 is accepted by Medicare, Medicaid, and many private insurers (coverage may vary by payer, but it is typically recognized as the standard PHP code). Providers use H0035 to claim reimbursement for each day a patient attends the PHP and receives the program’s full complement of services.
S0201 – Partial hospitalization services, less than 24 hours, per diem. This is an alternate code for PHP that some payers (often commercial insurers) use, essentially equivalent to H0035 in describing a PHP day of care. You will often see S0201 used for mental health PHP in private insurance billing, as it’s a code defined by certain payers for intensive psychiatric day treatment. Important: S-codes like S0201 are generally not accepted by Medicare or Medicaid. They are primarily for private insurance claims. In practice, some private plans prefer S0201 and others accept H0035 – your billing team should verify each payer’s preference to bill correctly. (Many providers default to H0035 for mental health PHP unless an insurer specifically requires S0201.)
H2036 – Alcohol and other substance abuse treatment program, per diem. This code is often used to bill day-treatment programs for substance use disorders, which can include PHP-like services for addiction treatment. In some cases, instead of using H0035, a substance-focused PHP might use H2036 to indicate a full day of structured SUD treatment (for example, if the payer wants to distinguish it from purely mental health programs). H2036 is common when payers want a per diem code for intensive outpatient addiction services. Sometimes, H0015 (which normally represents intensive outpatient for SUD, 3 hours) can be billed multiple units to cover a PHP day, but H2036 simplifies it to one unit per day. Always check the payer’s guidelines – some insurers require detailed breakdowns of services (using multiple codes for group therapy, individual therapy, etc.), while others allow a single per diem code for the entire PHP day.
Revenue Codes and CPT bundles: Hospital-based PHP programs (or PHPs in community mental health centers billing Medicare) may use APC (Ambulatory Payment Classification) bundling. Medicare expects PHP services to be billed with specific revenue codes (such as 0905 for intensive outpatient services, 0912 for individual therapy, 0913 for group therapy, etc.) on a UB-04 claim form, rather than a single HCPCS like H0035. However, for simplicity, freestanding programs often contract with insurers to bill using the above HCPCS codes. Ensure your billing software and team understand whether to bill a single per diem code or each service component. Behave Health’s RCM module, for example, can handle both scenarios and ensure claims comply with payer rules.
When billing for PHP, it’s essential to also append any required modifiers (for instance, modifiers for telehealth if the PHP services are provided via telemedicine, or HR modifiers if it’s a family session, etc., as required by the code). Also, keep in mind S9480 – this is the code for intensive outpatient psychiatric services (IOP, per diem), which is a level slightly below PHP. We mention it because some programs that offer PHP also offer IOP, and payers may only cover S9480 if the patient is in a less intensive IOP. Make sure you’re using the correct code matching the level of care authorized for the patient (PHP vs IOP).
Insurance Coverage and Reimbursement for PHP
Most major insurers – including Medicare, Medicaid (in many states), and commercial health plans – cover Partial Hospitalization Program services when they are medically necessary and provided by an eligible facility. Here are key points regarding reimbursement:
Medical Necessity & Certification: Insurers require that PHP be medically necessary, meaning the patient’s condition warrants daily intensive therapy but not 24-hour inpatient care. For Medicare, a physician must certify that the patient would otherwise need inpatient treatment if PHP were not available. The patient’s care plan must indicate a need for at least 20 hours of therapeutic services per week in a PHP. Likewise, private insurers will typically review clinical documentation to ensure the patient meets admission criteria for PHP, such as active psychiatric symptoms or relapse risk that cannot be managed at standard outpatient level. It’s common for insurers to require an initial authorization and ongoing concurrent reviews (weekly or bi-weekly) to continue approving PHP days.
Prior Authorization: Prior authorization is almost always required before a patient starts a PHP, especially for private insurance. For example, Blue Cross Blue Shield plans often require the provider to call a behavioral health case manager for approval prior to admitting a member into a PHP. Failing to get pre-authorization can result in denied claims. It’s best to verify benefits and obtain authorization for a set number of PHP days (e.g., 5 days at a time) and then request extensions as needed with updated clinical information.
Insurance Billing and Claims: When billing insurers, use the appropriate code (H0035, S0201, etc.) per day, and make sure to include documentation of the services rendered each day in case of audits. Some payers reimburse PHP at a fixed daily rate, while others may have fee-for-service components (for instance, paying separately for psychiatric evaluations or certain group therapies). Medicare’s PHP reimbursement (for hospital-based or CMHC programs) is bundled into a per diem rate that covers most services except physician charges. Commercial insurance rates for PHP can vary widely; as a provider, negotiate rates that account for the intensive resources PHP requires (staffing, facility costs, etc.).
Coverage Limitations: Despite mental health parity laws (the Mental Health Parity and Addiction Equity Act requires insurers to cover mental health care at levels comparable to medical/surgical care), PHP coverage can sometimes be limited by insurers. Historically, inadequate reimbursement and coverage gaps have made PHPs scarce in some regions. The National Association for Behavioral Healthcare notes that many regions lack PHP programs partly due to low reimbursement rates from Medicare/Medicaid and some commercial plans not covering PHP at all. However, this is improving with advocacy – Medicare now recognizes PHP as a distinct benefit and many ACA marketplace plans include it. Always check each payer’s policy: some may cap the number of PHP days, or require step-down to IOP after a certain time even if not fully recovered.
Patient Costs: Under Medicare Part B, patients in PHP owe the standard 20% coinsurance after meeting their Part B deductible (Medicare covers 80% of the approved amount). For private insurance, copays or coinsurance for PHP can vary; some plans charge a specialist visit copay per day, others treat it like an outpatient hospital service with percentage coinsurance. Ensure your admissions team communicates any out-of-pocket cost to patients upfront to avoid surprises.
Billing Compliance: Because PHP involves many services (therapy, med management, etc.), compliance is critical. Maintain detailed daily progress notes and treatment plans, as payers or auditors may request documentation to substantiate that each day billed met the PHP criteria (e.g., the patient participated in structured therapies for the required hours). If using a billing software like Behave Health, leverage features like automated charge capture and claims scrubbing to reduce errors. For instance, Behave Health’s RCM module can be configured to automatically use the correct revenue codes and ensure that only one unit of PHP is billed per day (some insurers have edits to deny multiple PHP claims in one day).
Internal Links: For more on billing, see our HCPCS/CPT code guides such as the deep-dive on H0035 Partial Hospitalization billing and S0201 PHP billing on the Behave Health blog. We also offer an Insurance Billing Guides section covering topics like coding, documentation, and tips for maximizing reimbursement. (For example, check out our complete guide to addiction treatment insurance billing in Florida to understand state-specific nuances and general best practices.)
Patient Experience and Benefits of PHP
From a patient’s perspective, a Partial Hospitalization Program can be a life-changing support system. PHPs provide a high level of care while allowing patients to remain connected to home and community, which offers several practical and clinical benefits. Below, we explore what a typical day in a PHP looks like and the key benefits of Partial Hospitalization Programs for patients:
Structured Daily Routine: Patients in PHP follow a structured schedule each day, which may run from roughly 9:00 AM to 3:00 PM (for example). Mornings might begin with a check-in group or mindfulness exercise, followed by various therapy groups, skills workshops, and possibly one-on-one sessions. Afternoons could include additional therapy (or specialized sessions like art therapy, movement therapy) and a wrap-up process group. This intensive structure is beneficial because it fills the patient’s day with therapeutic activity, reducing idle time that might lead to negative thoughts or behaviors. Especially in early recovery from addiction or during acute mental health episodes, maintaining structure is crucial. Patients often find that the routine helps them build healthy habits, restore sleep schedules, and provide a sense of purpose each day.
Staying at Home (or Sober Living): Unlike inpatient hospitalization, PHP patients do not stay overnight at the facility. They return home in the evenings, or some may stay in a sober living house or supportive housing if home isn’t conducive to recovery. This has multiple benefits: patients can practice the coping skills they’re learning in a real-world setting (home/work) each evening and weekend, which helps bridge the transfer of skills from treatment to daily life. It also means patients can maintain family relationships – for example, a parent can attend a PHP during the day but still have dinner with their children at night. This arrangement often reduces the family burden compared to full hospitalization, as loved ones can be part of the healing process more easily.
Intensive Therapeutic Support: PHP provides many hours of therapy per week (often 20+ hours), which can accelerate progress. Patients have the advantage of multiple therapy modalities: daily group therapy allows peer support and learning from others with similar struggles; individual therapy sessions (usually at least once a week in PHP) provide personalized attention; and family therapy sessions (commonly offered, if family is involved) help educate and involve support systems. The variety of groups might cover cognitive-behavioral techniques, dialectical behavior therapy (DBT) skills, relapse prevention planning, stress management, medication education, and more. The intensity and diversity of interventions in PHP have been shown to reduce symptoms quickly – for instance, studies have found significant reductions in depression and anxiety scores over a few weeks of PHP treatment, comparable to inpatient outcomes. By the end of a few weeks in PHP, many patients report feeling more stable, empowered with coping strategies, and better prepared to manage their conditions.
Medical Oversight and Safety: Even though PHP is outpatient, patients benefit from regular medical monitoring. Psychiatrists and nurses evaluate patients frequently. Psychiatrists in a PHP will typically see each patient at least once a week (and more often if needed) to adjust medications and assess risk. Nursing staff might check vital signs daily or as needed, and are on-site to handle any issues (for example, if a patient feels unwell or has side effects, the nurse can intervene). Having medical professionals available during program hours gives patients confidence that their health is being closely watched, and any warning signs of trouble (like escalating suicidal thoughts or withdrawal symptoms) will be caught early. In fact, PHPs often have protocols for emergency evaluation – if a patient’s condition deteriorates, the team can facilitate a direct transfer to inpatient care promptly. This safety net can prevent crises. The presence of a multidisciplinary team (psychiatrist, therapist, nurse, possibly a case manager) means comprehensive care – e.g., medication management is integrated with therapy so the whole team is on the same page regarding the patient’s progress.
Skill-Building and Transition Planning: A key focus in PHP is teaching practical skills for independent living and relapse prevention. Because patients return to their everyday environment after the program day, they can immediately practice what they learn. PHPs often include sessions on life skills, vocational rehabilitation, or social skills training. Some PHP programs (especially in mental health) might incorporate occupational therapy or employment support, helping patients gradually resume work or school. The treatment team works on a discharge plan from day one – planning the next steps for when PHP ends. This might involve setting up aftercare like step-down to an Intensive Outpatient Program (IOP) (which is usually 3 days a week) or arranging ongoing outpatient therapy and psychiatry appointments. The benefit here is that by the time a patient graduates from PHP, they already have a lower-intensity plan in place, minimizing gaps in care and reducing the chance of relapse or rehospitalization.
Peer Support and Reduced Isolation: Many patients start PHP after a hospital stay or during a mental health crisis where they feel very alone in their struggle. In PHP’s group therapy milieu, they meet peers facing similar challenges. Connecting with others in group sessions can reduce the stigma and isolation a patient feels. They gain support, can role-play interpersonal situations, and build a sober or wellness-focused network. Graduates of PHP often say one of the biggest benefits was knowing “I’m not alone” and learning from others’ experiences. PHP can foster a sense of community and hope, which is therapeutic in itself. Some programs also involve alumni activities or support groups for people who have completed PHP, to keep those peer connections alive.
Effective Outcomes: Partial Hospitalization can be very effective for the appropriate patients. Research has indicated that PHPs can achieve outcomes similar to inpatient care for many individuals. For example, one study of acute psychiatric PHP patients found that 92% of patients showed improvement by the end of the program and only 5% required readmission to inpatient care within 30 days (Predictors of Outcome of Acute Partial Hospitalization: An Exploratory Study). Patients often experience moderate to large reductions in symptom severity during PHP treatment (Predictors of Outcome of Acute Partial Hospitalization: An Exploratory Study). Additionally, the NABH notes that PHPs help prevent unnecessary hospitalizations – many people are able to stabilize in a PHP who might otherwise have been hospitalized if PHP were not available. By avoiding or shortening inpatient stays, PHP not only helps the patient avoid the disruption of hospitalization but also lowers healthcare costs (since outpatient treatment is generally less expensive than inpatient). Families also benefit when their loved one can recover in a less restrictive setting; they can observe progress and be part of family therapy sessions to improve understanding and communication.
Flexible and Personalized Care: PHPs often can be tailored to specific populations or needs. For instance, some treatment centers run specialized PHP tracks: a mental health PHP, a substance abuse PHP, a co-occurring disorders PHP, or even age-specific programs (like adolescent PHP or geriatric PHP). This means patients get a program more targeted to their situation, which can improve engagement and outcomes. Within a PHP, the treatment plan is personalized – if a patient is struggling with trauma, the therapist might incorporate trauma-informed care; if another has bipolar disorder, the groups might focus on mood management. The relatively smaller group sizes and close monitoring in PHP allow for adjustments as needed. If a patient is doing exceptionally well, the team might step them down to IOP sooner; if one needs more time, they can extend PHP a bit longer. This adaptability ensures each patient gets the optimal benefit from the program.
Overall, the PHP level of care offers a balanced approach: intensive treatment and the ability to practice living in the “real world.” Patients often emerge from PHP better equipped to handle daily stress, with a solid aftercare plan, and feeling hopeful about managing their mental health or sobriety going forward. The structure, support, and skills gained in PHP can significantly improve a patient’s trajectory, reducing the likelihood of relapse or crisis and empowering them towards long-term recovery.
Enhancing and Operating a Successful PHP Program
For healthcare providers and organizations, running a Partial Hospitalization Program requires careful coordination of clinical care, compliance, and operations. Success means not only helping patients achieve recovery but also managing the program’s business aspects effectively. Here are a few tips and resources for providers:
Stay Compliant with State and Accreditation Standards: As discussed, ensure you have the proper state licenses for PHP (whether in Texas, Florida, California, or elsewhere) and adhere to regulations on staffing, safety, and patient rights. Consider obtaining accreditation from bodies like The Joint Commission or CARF for your PHP, as this can strengthen your program’s quality and is often required for insurance contracts. (Behave Health can help direct you to resources for licensing and accreditation – for example, pointing you to consultants for Joint Commission or CARF accreditation if you need assistance (How to Turn Your Group Practice into an Outpatient Addiction Treatment IOP or PHP Facility in Florida — Behavehealth.com).)
Optimize Your Billing and RCM: Given the complexity of PHP billing (authorizations, daily billing, utilization reviews), having a robust revenue cycle management system is essential. Behave Health’s all-in-one platform, for instance, integrates EHR clinical notes with billing, so all services documented can flow into claims with the correct coding. Automation can ensure you don’t miss billing for a day of PHP or accidentally bill when the patient was absent. Our software also helps manage insurance authorizations and track utilization, alerting your team when re-auth needs to be requested. Efficient billing not only improves cash flow but also frees your staff to focus on patient care instead of paperwork.
Leverage Internal Resources and Guides: We at Behave Health have compiled numerous guides and articles to help PHP and IOP programs thrive. If you’re just starting out, read our state-specific startup guides (like the Texas and California guides mentioned earlier) to avoid common pitfalls. For billing teams, explore our Insurance Billing Guides repository – e.g., learn about the top billing codes in your state (see our article on most used addiction treatment CPT codes in Texas for an example of how coding varies by region) and our comprehensive guide to behavioral health billing and coding that covers best practices and common mistakes. Continuous learning and staying updated on coding changes (like CPT/HCPCS updates each year) will keep your PHP financially strong.
Engage Patients and Encourage Feedback: A great PHP program continuously improves by listening to patient feedback. Implement patient satisfaction surveys or alumni focus groups. Satisfied patients become advocates for your program (referrals via word-of-mouth), and their insights can help you fine-tune the curriculum or environment. Perhaps patients want more trauma-focused groups, or they suggest having family days on weekends – you can adapt to meet their needs better than competitors. Additionally, engaged patients are more likely to complete the program, improving your outcomes and metrics.
Promote Continuity of Care: Collaborate with referral sources and aftercare providers. Build relationships with inpatient units (they can refer patients to your PHP upon discharge) and outpatient therapists (so they trust discharging their clients to your PHP and getting them back after). Creating a seamless continuum – inpatient -> PHP -> IOP -> outpatient – with warm handoffs in both directions will position your program as a trusted part of the community’s behavioral health network. This not only benefits patients but also can be a selling point to payers and health systems.
Finally, remember that running a PHP is a significant undertaking, but you don’t have to do it alone. The right partnerships and tools can streamline your operations immensely.
Ready to enhance your PHP program’s efficiency and outcomes? Behave Health is here to support you. Our all-in-one software platform is designed specifically for behavioral health providers, including PHPs and IOPs, to simplify everything from clinical documentation and scheduling to billing and insurance claims. We also provide business intelligence to track your program’s performance and ensure compliance at every step. Contact us for a consultation to discuss how we can help your organization, or get your free trial started today and see why more treatment centers prefer Behave Health. Whether you’re launching a new PHP or looking to optimize an existing one, our team and tools will help you deliver high-quality care while maximizing efficiency and reimbursement.
(Interested in learning more? Download our free guide on behavioral health billing or browse our blog for more insights into running successful treatment programs. And as always, if you have questions, feel free to reach out – we’re passionate about helping behavioral health providers succeed in their mission to save lives and improve communities.)