Wondering how to get your addiction treatment center started with registration and network registration for Florida Blue?
Today, we’ll look at why you’d want to register with Florida Blue, what it takes to get registered with Florida Blue, as well as the difference between registration and joining the Florida Blue network as an addiction treatment provider.
What Do Addiction Treatment Centers Need to Know About Florida Blue?
Florida Blue is a member of the Blue Cross Blue Shield Association based in Florida. Because BCBS acts as a type of franchise, Florida Blue essentially operates as an independent company that pays to use the BCBS name and other identifying assets. Florida Blue is owned by a larger insurance company called Guidewell, who is, itself, the 10th largest insurance payor in the United States.
How Does Behavioral Health Care and Addiction Treatment Work at Florida Blue?
Florida Blue contracts with a managed behavioral health network called New Directions Behavioral Health for all of its behavioral healthcare needs, including addiction treatment. You can be registered with Florida Blue directly without going through New Directions Behavioral Health but in order to be considered an in-network addiction treatment provider with Florida Blue, you must join New Directions’ network as a provider.
Getting Registered with Florida Blue As an Addiction Treatment Center
Registering with Florida Blue is the first step to becoming an in-network provider. Without registering, you will not be able to collect any reimbursements for any claims submitted to Florida Blue. You will simply not exist in their system without registration.
In order to register with Florida Blue, you will need to obtain an Availity Essentials account or log into your existing account, as most paperwork is handled electronically for Florida Blue through Availity, including new provider paperwork. Availity is an EDI (or electronic data interchange) that helps sync up data between two different parties that’s experienced runaway growth in recent years.
Registering with Availity Essentials is completely free. All you have to do is complete the Availity Essentials visit their registration page.
Becoming an In-Network Addiction Treatment Provider with Florida Blue
Becoming an in-network provider with Florida Blue is significantly more complicated than simply registering with Florida Blue.
There’s several reasons for this added layer of complexity.
1 - All behavioral healthcare is managed for Florida Blue by a third party, New Directions.
2 - Instead of completing a request to join Florida Blue’s network, you’ll be required to submit a request to join New Directions’ network.
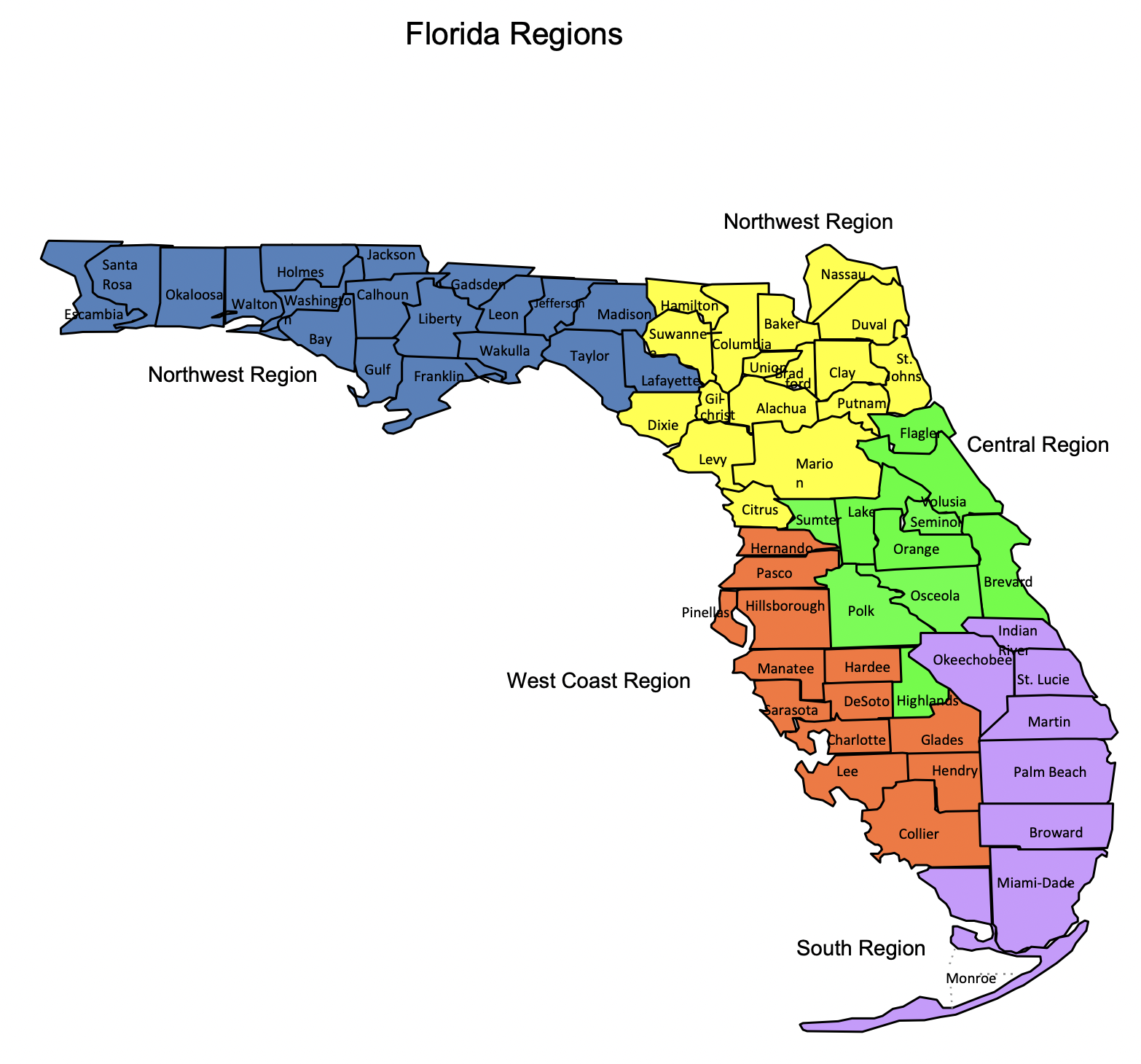
3 - You may only join the New Directions network if the “network status” reads as “open” on Florida Blue’s network status table. As of this writing, the network status for all would-be addiction treatment providers in network with Florida Blue is “closed.” That means that Florida Blue (and New Directions, by extension) is not accepting new providers at this time. The network status table is known to change from time to time, so Florida Blue encourages you to check back periodically to see if there’s any in-network openings under behavioral health.
When you’ve found that the network status table reads “open,” you may then submit a request to join New Directions’ (and Florida Blue’s) network.
Trouble With Addiction Treatment Registration with Florida Blue? We Can Help.
BehaveHealth’s Revenue Cycle Management (RCM) service includes soup-to-nuts, hyper-detailed, hands-on attention to every single component of your addiction treatment billing needs. We have strong working relationships with every major insurance company in the United States.
Even better, we’re not health care generalists. We only work for behavioral health providers like you.
Let our team of specialists handle it all:
Verification of Benefits
Utilization Review
Billing and Collections
Patient Responsibility
Denials and Appeals
Get your free trial started today and see why more addiction treatment centers prefer Behave Health.